Dr. Megan Anna Neff and Dr. Debra Brause on the Complex Relationship Between Traditional Therapeutic Modalities and Neurodivergence

This episode has been a few months in the making and it’s on a topic I’m personally very interested in and I feel like not enough people are talking about — and that topic is, the intersection of traditional therapeutic modalities and neurodivergence. Specifically, I wanted to examine how some therapies may not meet the unique needs of neurodivergent individuals and what it means for a therapist to be truly neurodivergent-affirming. And I have two wonderful guests to get into it with me — Dr. Megan Anna Neff and Dr. Debra Brause.
In this conversation, Megan Anna, Debra, and I explore what some limitations and challenges are for neurodivergent clients working with therapists who don’t understand their neurotypes, how therapeutic approaches can be adapted to provide sensory safety and center the client’s experience and agency, why cognitive-behavioral therapy (CBT) and dialectical behavior therapy (DBT) may not be as effective for differently wired people, as well as the potential limitations of standard strategies like mindfulness and visualization as. Most importantly, we’ll discuss the qualities to look for in a therapist who is truly neurodivergent affirming —what that means, and how it can make all the difference in a child’s therapeutic journey.
About Dr. Megan Anna Neff
 Dr. Megan Anna Neff (she/they) is a neurodivergent Clinical Psychologist and founder of Neurodivergent Insights where she creates education and wellness resources for neurodivergent adults. Additionally, she is co-host of the Divergent Conversations podcast. As a late-diagnosed AuDHDer (Autistic ADHD), Dr. Neff applies their lived experiences from a cross-neurotype marriage and parenting neurodivergent children to their professional focus. They are committed to broadening the mental health field’s understanding of autism and ADHD beyond traditional stereotypes. This personal-professional blend enriches their work and advocacy within neurodiversity.
Dr. Megan Anna Neff (she/they) is a neurodivergent Clinical Psychologist and founder of Neurodivergent Insights where she creates education and wellness resources for neurodivergent adults. Additionally, she is co-host of the Divergent Conversations podcast. As a late-diagnosed AuDHDer (Autistic ADHD), Dr. Neff applies their lived experiences from a cross-neurotype marriage and parenting neurodivergent children to their professional focus. They are committed to broadening the mental health field’s understanding of autism and ADHD beyond traditional stereotypes. This personal-professional blend enriches their work and advocacy within neurodiversity.
Dr. Neff is the author of Self-Care for Autistic People and a forthcoming book on Autistic Burnout. Additionally, she has published in several peer-reviewed journals on topics ranging from neurodivergence, place attachment, relational psychoanalysis, social psychology, and integration of spirituality into psychotherapy. Passionate about distilling complex research into visually accessible formats, she translates research into visual pixels which you can find on her website, Instagram, and digital workbooks. Additionally, Dr. Neff is passionate about community building and creating digital communities by and for neurodivergent individuals.
About Debra Brause, PhD
 Debra Brause, PhD is a licensed psychologist and therapist who works from a neurodivergent-affirming stance, helping couples embrace who their children are, and providing support and guidance through this unique journey. Her professional training includes diagnostic assessment for learning disabilities at the UCLA Office for Students with Disabilities, and clinical work in community mental health settings including The Southern California Counseling Center and the Maple Counseling Center. She also received two years of training at the Wright Institute Los Angeles where she completed a postgraduate fellowship in psychoanalytic psychotherapy.
Debra Brause, PhD is a licensed psychologist and therapist who works from a neurodivergent-affirming stance, helping couples embrace who their children are, and providing support and guidance through this unique journey. Her professional training includes diagnostic assessment for learning disabilities at the UCLA Office for Students with Disabilities, and clinical work in community mental health settings including The Southern California Counseling Center and the Maple Counseling Center. She also received two years of training at the Wright Institute Los Angeles where she completed a postgraduate fellowship in psychoanalytic psychotherapy.
Debra received a B.A. in English from the University of Pennsylvania and continued her graduate studies with a Masters and Doctorate in Psychology from the California School of Professional Psychology (CSPP). CSPP is accredited by the American Psychological Association and is a multicultural program designed to train psychologists to work as clinicians with diverse populations. Prior to becoming a psychologist, Debra pent ten years in the entertainment industry, working in television production, news, and as a studio development executive. Her work with writers crosses into her therapy practice as she helps to move through psychological blocks and provide guidance toward finding one’s ideal creative path.
Things you’ll learn from this episode
- Why traditional therapy may not meet the needs of neurodivergent individuals
- How emotional regulation strategies might be adapted to provide sensory safety as a foundation for regulation
- The role of “goals” in therapy with adolescents and the importance of centering client experience and agency
- Ways in which CBT and DBT may not be as effective with differently wired people
- What the potential limitations of mindfulness and visualization as therapeutic strategies are in some neurodivergent clients
- Qualities to look for in a therapist who is truly “neurodivergent affirming” (as well as what that actually means)
Resources mentioned
- Self-Care For Autistic People by Dr. Megan Anna Neff
- Dr. Megan Anna Neff on Diagnoses and Misdiagnoses (Tilt Parenting Podcast)
- Reframing Autism: A Psychoanalytic Journey Towards Mutual Recognition (article on Neurodivergent Insights website)
- Why Doesn’t Standard Talk Therapy Work for Autistic People? (Dr. Alice Nicolls)
- How CBT Harmed Me: The Interview that the New York Times Erased (Disability Visibility Project)
- Kelly Mahler on Understanding and Supporting Kids’ Interoception Experience (Tilt Parenting Podcast)
Want to go deeper?
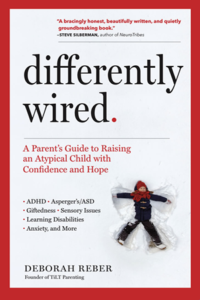
The Differently Wired Club is not your typical membership community.
 There’s something here for everyone, whether you’re a sit back and absorb learner, a hands-on, connect and engage learner, and everything in between. Join the Differently Wired Club and get unstuck, ditch the overwhelm, and find confidence, connection, and JOY in parenting your differently wired child.
There’s something here for everyone, whether you’re a sit back and absorb learner, a hands-on, connect and engage learner, and everything in between. Join the Differently Wired Club and get unstuck, ditch the overwhelm, and find confidence, connection, and JOY in parenting your differently wired child.
Learn more about the Differently Wired Club
Episode Transcript
Debbie:
Well, hello, Megan Anna and Debra. Welcome to the podcast.
Debra Brause:
Thank you. So happy to be here.
Debbie:
I am so happy to be here as well. And Debra, I’ll just say thank you, first of all, for reaching out to me and suggesting this conversation. I think this is gonna be one of those really interesting dialogues that we’re gonna have and talk about things that I don’t think are being talked about, at least in my parenting community, but frequently. So I’m hoping this is the start of a conversation that we’ll just continue having. But, I guess I’ve already read your formal bios. I don’t want to spend a lot of time here, but I would love it if you would take a moment and share your kind of personal interest or stake in the conversation we’re about to have today. And Debra, since you reached out to me first, why don’t you start?
Debra Brause:
Yeah, I mean, primarily I’m the mother of a 17 year old who’s an autistic ADHD-er. So that’s my coming in with that motivation of feeling very protective of that community. And I’ve been a psychologist for 20 years now. So the majority of my practice is parents of differently wired kids, autistic adults, a bunch of ADHD-ers and everyone else, lots of Hollywood folks. So my training did not prepare me at all to work with autistic clients. And that’s why I am trying to learn as I go and build my own neuro-affirming practice. And I’m just really motivated to share as I learn because I want to motivate my colleagues, clinicians around me to join me in kind of getting more education around this, creating a welcoming space, and being able to recognize neurodivergence even when it comes into our office. Because I think we’re not even trained to see it. And knowing the harm of not being diagnosed, I just think it’s so important that we educate ourselves. And so I am really trying to bring some education to psychology students that I’ve been working with, as well as just putting the word out for all of us to kind of be more aware of what autism looks like and how we can create welcoming therapy spaces for our autistic clients.
Megan Anna Neff:
Yeah, I feel like I have kind of two, like a foot in two worlds here. One is as a client, so I’m autistic ADHD. And like most of us have had mental health struggles my whole life. So I’ve, I’ve been to various therapists. And it wasn’t until I found a very kind of specific therapist that therapy really clicked for me. And so my initial thoughts were just my experience as ND then on the other side, as a psychologist, as a clinician, I’ve always adapted therapy, even before I knew I was autistic, I realized I was always adapting how I did therapy to work with my brain. But then more so as I’ve now specialized working with autistic ADHD adults and see how much needs to be adapted. And similar to Debra, that’s not something we’re trained in, which, you know, on the, that can cause a lot of harm in the sense that, like one thing I hear a lot from our community is they perhaps will disclose this identity to a therapist and they’ll say, I’m sorry, I don’t feel prepared to work with you. And I understand why clinicians are saying that because we’re also trained to work within our scope of practice. And this is frankly not in the scope of practice of mental health therapists. So kind of both sides as a clinician, as a parent, as a just neurodivergent human, and then as a therapist. I’m also interested in this conversation.
Debbie:
Yeah, that’s great. And I’ll share my personal stake in this and why I was so excited. Debra, when you reached out to me and said, hey, I’ve been thinking a lot about this and have you considered doing an episode on it? As the parent of an odd ADHD-er who has been in therapy, different therapies for a number of years, I have just noticed, and my child’s now a young adult, over the last few years, I’ve started getting really curious about the limitations of certain modalities that we were engaged in, that they were engaged in. And I just started to really question, wait a minute, you know, I started noticing red flags. And in conversations with my child, realizing, oh, they don’t really get who my kid is at all. And so I started reaching out to people and talking about it. And I’m still learning. And so I’m I’ve been learning from both of you and your writing and the voices that you have in this space. But I think just to have a conversation, not that we’re going to be fixing anything. This is a different episode as we talked about than a lot of my episodes of A Tour Like. Here are some strategies that you can take away. We will be sharing some things to think about when vetting therapists. But I see this as more of an exploration and kind of see where the conversation is right now in terms of neurodivergence and therapy. So I guess even to start, that’s where I would like to begin is just this conversation we’re having today. How new is it? Like who is talking about this stuff? If anyone, like is this something that is building a lot of momentum within the therapeutic provider space?
Megan Anna Neff:
I think so. I’d be, I’ll be curious to your thoughts, Debra, but I think so. And I want to do a shout out to Joel Schwartz, who, as far as I know, coined the term neurodivergent affirming therapy, or the first one to apply that concept to clinical work. And goodness, I think it might have been like 10 years ago, maybe it was eight years ago. And you can find a lot of vibrant communities, especially on Facebook, of neurodivergent affirming providers. So in one sense, yes, I think this is something that especially in the last five years has really expanded. At the same time, if you go, and I always have to remind myself, we live in a world where we live in so many echo chambers, and that’s my world. And then maybe I’ll go to a traditional mental health training program, and they’ll be like, what? So it’s really interesting if you are interested. There are absolutely places where clinicians can go and find community and trainings. But it’s not yet mainstream in many traditional training programs. So I would say the answer is yes and no.
Debra Brause:
I love that you’re doing the positive framing of things like where we can learn how to be neurodiversity affirming. Because yeah, what I’ve seen more of the Facebook communities where people are talking about therapy abuse, and you know, there’s one called Stop DBT, and people who are getting on really just kind of sharing their trauma around health, certain types of therapy have affected them. And so I’ve seen it mostly through, I mean, not just autistic people, but a lot of autistic self-advocates and where it just this whole issue is becoming more public and people, as autistic people are getting out there with their voice and being able to advocate, they can talk about the therapeutic experiences they’ve had. But yeah, finding those people who are creating and trying to implement a neurodiversity affirming practice that I’m seeing a lot. And it’s a matter of how deep it goes. I think a lot of people are calling their practice that, but then you’ll read their website and they’re doing things that are clearly not aligned with that. And so I think it depends on what it means to them.
Megan Anna Neff:
I’m so glad you brought that up. I was hoping to say that, because I love that the neurodiversity movement is taking off. But one of the drawbacks is people are now just stealing the language at a surface level and slapping it on their website. There’s actually a clinic, oh my gosh, I can’t believe I’m sharing this story publicly. There is a clinic that advertises being neurodivergent affirming… They stole my graphics as an autistic psychologist and a lot of my copy from my website, all very affirming. And then I looked at their other blog posts and it’s like ASD, but it’s like you’re advertising as neurodivergent affirming, stealing from creators. And like, so that would be the worst case. But there’s a lot of people that are just slapping the language on of we’re neurodivergent affirming. And you go deeper and it’s like, no, you have no idea what this framework actually is. You’re just, and then it’s like deceptive.
Debra Brause:
Unreal.
Megan Anna Neff:
And that’s what, like, obviously my, my arousal, my energy just went up because that’s, that’s what makes me really angry is when people are using it as a marketing strategy and aren’t understanding what it actually means to be neurodivergent affirming in their clinical work.
Debbie:
Yeah, I’m really happy that you all mentioned that too. I had made a note of that. That language, it does seem to be co-opted in some ways. And I think part of that is because of the speed with which the Neurodiversity Movement has been picking up. And I think people are eager to kind of, now that it has so much momentum, to kind of get behind it. But a lot of people don’t have a true understanding of what that actually means. And so I guess I’ll just say that with some of the providers that our family worked with I Start I spent a lot of time sending articles like Educating like oh you have never heard of rejection sensitive dysphoria well, let me share an article because this is a huge thing that is impacting my kid that you need to be aware of and a lot of the things that I shared weren’t necessarily, like I don’t think I ever got like, oh thanks, this is so interesting, I’ll check it out. I don’t think I got that response if I got any response at all. And so I’d love to kind of know, are there two camps here? I don’t know if camps is the right word. I’m just wondering in terms of the majority of therapists who kind of, they go and they get their training and their degree and they hang up their shingle and they start working with people with, you know, anxiety, depression, mood disorders, all of those things, especially that a teenager or young adult might be struggling with. How many people kind of even have an understanding and is there, do you notice a lot of resistance in openness to the neurodivergent experience?
Debra Brause:
I mean, I can answer that from a, I’m in the psychodynamic world, which Meghannan has been in as well, but I belong to lots of peer supervision groups where I bring this information into my colleagues and some of them are open and very curious and others I think dig their heels in a bit of like they’ve been trained to see things a certain way. There is as benevolent and wonderful as psychoanalytic type therapy can be. There’s also kind of a pathologizing eye, I want to say, where we’re interpreting things through a certain lens that you’re looking for the client’s defenses. You’re looking at their character, logical issues, and maybe kind of, um, I’ve seen people sort of double down on their conceptualization of a client and not really being willing to see where neurodivergence might play a part and how something that they’re assuming is a defense of some kind is actually a neurodivergent trait. And so I think it depends on the person and how open they are to kind of learning and exploring versus like this really hardcore stance where people are married to their discipline and really not willing to open their mind to new information. But be curious what Megan Anna has to say.
Megan Anna Neff:
Thank you. I, yeah, I’ve talked about this kind of from the beginning of my discovery, because that was why I started neurodivergent insights. I was like, how do I have a doctorate? And I’m just learning this about my kid and myself. So we talk about confirmation bias a lot in psychology, which is that when we have a theory in mind, our mind naturally looks for data to support that theory. And sometimes I think it’s meant to health professionals. We forget we have confirmation bias. And as a field, we do across the board. We’ve done a lot of really fantastic work in trauma in the last 20 years. And that work is so needed and so meaningful and it’s helped so many people heal. However, it’s become a little bit of a confirmation bias. We are primed to see trauma. So if we’re seeing someone with attachment stuff, someone with sensory stuff, someone who intimacy is uncomfortable for them, someone, a lot of these things will get interpreted as trauma. I’ve encountered countless women and non-binary people for whom their therapist told them it was trauma, not neurodivergence. And so I think that’s one of the places the field at large is really missing neurodivergent people, especially women and genderqueer people and people of color, where the default is often, well, this is trauma. And it’s not either or, it’s often both, frankly. But the trauma overshadows the neurodivergence.
Debbie:
It’s so interesting because I have experienced where I was trying to explain that most if not all neurodivergent people have some trauma because of being neurodivergent in a neuro typical world and I’ve gotten pushback. Well, this isn’t actually trauma. This is the depression or things, so it’s interesting to hear that your experience has been that often the trauma takes precedence.
Megan Anna Neff:
So I think I understand where some clinicians might be coming from with that comment. One framework that’s been really helpful for me comes from Kelly Mailer, who talks about atypical trauma. So things like sensory trauma, social based trauma. There’s also another really interesting article that looks at why, specifically why autistic people are more prone to develop PTSD after a traumatic experience, even when they don’t meet criteria A. I realize I’m getting really clinical, but criteria A are kind of the classic, are the classic things that we have as a society have deemed big T trauma. Autistic people are more prone to develop PTSD even when they don’t meet criteria. And there’s a lot of reasons for that. One of that being, you know, our more sensitive nervous system, the way we encode things on a sensory level, some of our cognitive style. So I could see why a clinician might be like, well, that doesn’t sound like classic trauma, because often we do have atypical trauma and atypical trauma responses.
Debra Brause:
There’s so much overlap too as you’re talking about. So it’s so hard to tease out what’s the trauma and what’s the autism or neurodivergence. And it’s like people want to put you in one box or the other. And so that overlap of the two is confusing for people. And to be able to consider both is obviously really important that they might be both well, they’re always both there really on some level. So but it doesn’t mean that one when we, they’re not mutually exclusive. So I think it’s just someone who’s open to how these two things intersect.
Debbie:
Yeah, thank you. So I want to start talking about some of the limitations or potential challenges or maybe, you know, harmful impacts of some therapies with neurodivergent people. Okay, so I would love to if we could start talking about what some of the challenges are and maybe we could start if you could each share things that you particularly have noticed or been thinking about as therapists in ways that some modalities and we don’t have to get into specifics yet unless you want to in terms of specific modalities, but in the ways that they may not meet the needs of their neurodivergent clients. So, I don’t know … whoever wants to start.
Megan Anna Neff:
I’ve got two thoughts, okay, I’ll start. Okay, so I guess the two thoughts that popped into my head right away, one has to do with kind of access to our inner world. And this is why therapy, especially as someone who’s moved through the world. How do I, I don’t know, I never know how to say this. I identify as agender. So move through the world as a primarily culturally socialized as a girl. And that’s how my therapists have treated me. Where there’s a lot of expectation around like emotions and like the warm gooey stuff. And I’ve never been like, oh, that feels intrusive. It feels, I don’t connect to it. So whenever therapists, and this goes back to what Debra was saying earlier about how like a tendency to see things as defenses. I let people into my inner world through my mind, through ideas, through philosophy. So I might bring in like a really rich metaphor, something I’m reading on, but then a therapist might try to redirect me to my emotions, right? Of like, yes, but how do you feel about that? Which is turning what I’m doing as an object-based conversation, which is a very autistic way of communicating the inner world, but through a medium. And then the therapist is flipping it into a social based conversation, which is that’s all that tells me about yourself, who are you? Those all feel like sensory demands to me. And they are very hard to answer because it requires complex synthesis of things. Like, how am I like if you were to ask me right now, Debbie, like, how am I? I don’t know, like, what bucket of my life are you talking about? How am I going to synthesize all that information? That both simultaneously kind of freezes me up in a freeze response and also feels intrusive. And a lot of therapy is geared around getting at emotions and seeing the intellectual as a defense.
So I think that the biggest thing is actually taking the mind seriously. And that’s when I found a therapy that finally worked for me with someone who, we didn’t know I was autistic, but he took my mind seriously and let that be the access point for how I introduce my inner world. The second big thing I would just say is the sensory piece. We aren’t trained about interoception. We aren’t trained about sensory systems for the most part. So I know for me, like I learned a lot about how to teach emotional regulation strategies. But if you’re trying to teach an emotional regulation strategy on top of a dysregulated sensory system, it’s not going to go well. And I think the client’s going to feel like I’m failing at this. Nothing works for me. often feel more defeated. The therapist might start to feel frustrated and helpless. And it’s because there’s this huge piece, a foundational piece of the regulation system that’s missing. So those would be two things, two areas where I see therapists unintentionally missing, especially autistic clients.
Debbie:
And before you jump in, Debra, I just want to clarify emotional regulation strategies. Can you give us an example of one that wouldn’t be attuned to a sensory experience?
Megan Anna Neff:
So I mean, emotional regulation strategies might be like, um, deep breathing, grounding, self-compassion statements, cognitive reframing, these are all good things. Um but if I am emotionally dysregulated because the lights are cause like the lights are causing overwhelm or because I’m not moving my body because I’m repressing it, I might take a deep breath but it’s not really going to do much until I can get sensory safety and until I can use sensory inputs. I’m not saying those practices aren’t helpful, they are, but they often I think more foundationally is cultivating that sensory safety.
Debbie:
Thank you. Okay. Thank you for that. How about you, Debra?
Debra Brause:
I just want to add to that because I’ve learned so much from Meg and Anna describing these things and kind of bringing it into my practice. And in line with that, when clients are talking about something that’s a special interest for them or something that they’re truly passionate about. And I just had this talk with a friend last night who I think the therapists I know feel like if someone is going on and on and on about something that they love, that we are supposed to kind of rein it in, like interpret it, give them something maybe more practical or make meaning out of it. And they’re not realizing that this is a truly deep way of connecting, that their emotions are part of what they’re talking about. It might sound intellectual, but it is. I love Megan Anna’s words about how thoughts are confused with emotion. And so it can be very shaming, I think, or very just not helpful to try to cut someone off or take away something that they’re sharing that is deeply meaningful to them. And so just to be aware, I think we’re so afraid that we’re not being helpful, but that actually it is so helpful to just be able to join someone and be in that experience with them and share it and have them feel like seen and understood is the therapy, I think. And so I just wanna amplify that part.
I mean, for me, a lot of the stance of the therapist is so critical, like when we’re that kind of medical model where, you know, this person comes in and we’re meant to like, treat them, you know, and that sort of philosophy is so harmful. And that when we approach people with humility and with curiosity about their experience like that to me is like. Those are keywords for me of like, how do I approach this person and try to understand them and who they are and how can I help them understand themselves? But that I am not the I’m not the holder of truth. I’m not the person who’s going to tell them who they are or how they should be. Because I have my own ableism that I’m not aware of, right, of how I think people are supposed to behave. Like how I was taught, traditional therapy is coming from an ableist place. It’s this sort of normative psychology. And so to be really humble about how other people experience the world and help them get to know themselves without assuming that I know what health is, right? It’s so variable. And so yeah, I think we do harm when we assume that we know better or when we take a pathologizing lens on a person based on our assumptions.
Debbie:
So as you were talking about that, this idea of having an agenda came up for me. And I also just want to clarify, you know, we have listeners of kids of all ages here and I think it’s different. And tell me where I’m wrong here, but I think it is different if we’re talking about adults who are kind of willingly going into a therapeutic relationship versus an adolescent, like a teen or a young adult whose parents, you know, are trying to get them support and who may be struggling with mental health. Maybe that is what kind of brought them into therapy in the first place. And something that I think a lot about is exactly that. The holder of truth is kind of top down. Like the therapist has an agenda, the therapist has goals and a plan. And I love to explore that a little bit, like who, with a younger person who may be showing up to therapy because somebody else wants them to be there. Can you talk about that dynamic and the goals? Who’s setting the goals?
Debra Brause:
I mean, yeah, it’s so interesting. I mean, for me, the parents may come in with goals, right? But that doesn’t mean, I feel like that falls away as soon as you’re in the room with the client. And a lot of the work might be educating the parents around like what you’re actually working on and that maybe their goals are totally valid and things to be reflecting on, but ultimately it’s building that rapport and that relationship with the client and understanding what they’re needing. And those goals will either be relevant or not. Sometimes they’re looking from the outside in and that maybe they’re looking at behavior, right? And not understanding that there is like a whole context to that behavior and a meaning that is actually gonna shift once that person feels understood. So I think that goals have to be really flexible. And it might be a lot of psychoeducation with the parents about like, we’re not just looking at symptoms here, we’re creating a relationship where I’m going to understand your child and work with them to really feel through what they’re needing. And it might not be what we set out to do. What do you think, Megan Anna?
Megan Anna Neff:
I have lots of thoughts, lots of divergent thoughts. One, I just, as a therapist, it’s really hard to work with a youth or young adult when they’re there because their parents want them to be there. I actually often will not recommend, if a parent reaches out, I’ll say wait till your child expresses interest. When they do come in that way, I’ll often pivot really fast to like, okay, so your parents want you to be here, or like what are your thoughts about that? Because I just think any treatment, especially with neurodivergent people, is going to be pretty hard when the child doesn’t want to be there. I think one of the dynamics that often shows up for neurodivergent people is people are trying to fix me and it’s so easy to then reenact that in the therapy when it’s when the child doesn’t have a desire to be there, um, that they are able to, um, anchor into. And that’s whether I’m working with youth or adults, like I’ll be really explicit about that of, hey, there’s probably, I’m imagining you’ve kind of fallen into this dynamic of like, maybe people trying to fix you. And I really want to have an eye on not repeating that here. And sometimes that can be hard because sometimes people will pull for like, fix me, fix my executive functioning challenges, fix this. And then we’ll talk about it when it shows up of like, okay, I’m getting a fix it energy, what’s happening here. So I just think being aware is something that happens a lot to us and that can often get repeated, especially if we’re not the ones initiating therapy. So I just don’t think treatment’s very effective unless the goal is coming from the person, himself.
Debbie:
Yeah. Yes, agreed. And there are so many parents listening to this who are like, my kid is struggling, is not thriving, and they need therapy. They need, you know, so that is, go ahead.
Megan Anna Neff:
So this is, and this came up, and we just recorded a podcast and you asked about PDA, which of course I had like so many thoughts afterwards, but this is, and again, it’s gonna depend on the situation and if someone’s in crisis, right? This is where, like if one of my children is not doing well, it might be like, okay, we know that these are five things that are good for your mental health and your body. Like walking and moving your body every day. There’s a lot of research about what that does to neurotransmitters, therapy, like, and giving a menu of options to, again, reclaim the agency. So that’s one thing I do as a parent, a lot of, here is the menu of options of things that are good for your mental health. Where can I get some buy in from you? We’re going to do one of them, which one is the most tolerable? And because yeah, absolutely. Like a lot of our kids are struggling with mental health and falling into unhelpful patterns. And so I think however you can get buy-in to do some intervention is going to be really helpful.
Debra Brause:
Well, I was just thinking like it’s there’s no intervention that’s going to work unless they feel safe and unless they feel like they’re they’ve built a trusting relationship with you. So you can have all the goals in the world, but you know, unless you’re actually creating a relationship where someone wants to be with you and feels like you are on their side, helping them like nothing’s going to work anyway. So I think the more we try to come in with an agenda, it’s just going to backfire. So I think you have to just really hold the agenda lightly and really work on the relationship first.
Debbie:
So I think what we’re doing is we’re kind of talking a little bit about an ideal situation and what we as parents and caregivers should be looking for in a therapist or who’s working with our kids. So I just wanna put that out there. And I wanna also just acknowledge that I think that is not the majority of the providers that are working with our kids. So we’ll spend a little more time at the end of this conversation talking about some things to be really keeping an eye out for when looking for a therapist for our kids. But I just wanted to kind of, we’re talking about an ideal scenario. It is starting that relationship, the child is invested and willing, a willing participant in this and the therapist is coming in prioritizing connection and the client’s goals. I want to talk a little bit more about a couple modalities, specifically CBT and DBT. So we won’t go too far down the rabbit hole in this, but I do want to just touch upon CBT and DBT, so cognitive behavioral therapy and dialectical behavioral therapy. Those are kind of very common modalities. They are based on, and you guys are the experts, but my understanding is it’s based on really thinking about how your thoughts control, you know, impact your emotions and how we can change our thoughts so our emotions feel better. So I’d love to just spend a few minutes talking about those modalities and how they may or may not be as neurodivergent-affirming as we would like, because I have experienced and seen those particular techniques not be super beneficial.
Megan Anna Neff:
I’ll take CBT if you want to take DBT, Debra.
Debra Brause:
Sure.
Megan Anna Neff:
So with CBT, it’s so interesting because like, it’s often praised as the gold standard for autistic people, I think, because the idea is like, oh, autistic brains are so logical that this will work so well. Um, and I do want to say there are some CBT providers out there who are contextualizing it really well, but whenever you’re working with a marginalized group, you just have to be so thoughtful about what you’re doing. So a lot of CBT, it is about the fact, you know, the thoughts we’re having influence our emotional response to it. So like cognitive reframing, and that’s where it’s reframing an experience we’re having. That’s kind of a core part of CBT. So for, let’s take an example of a child who goes to school and they have the thought like, everyone’s looking at me and no one likes me, right? And then they take that to therapy. And then the therapist might, let’s work with that thought. What’s the evidence that no one likes you? Well, maybe there’s a ton of evidence don’t like that child and maybe they’re getting, maybe there’s a lot of those moments of disconnection from their peers, that’s going to be really invalidating of that experience and it’s not contextualizing that person’s experience as a neuro minority and what their experience is. And so if CBT is being done without taking that broader lens of what is this person’s reality, it can feel really invalidating and frankly just not be very helpful. The other thing I will sometimes notice with those of us with really divergent brains when we start getting into an argument with our thoughts, sometimes it makes us go deeper into the wrestling of like, oh, okay, maybe that’s not true. But then we have a counter argument, because our brains are just so divergent that then we go deeper into it and get more stuck. I am a proponent of third wave CBT, which is so like acceptance commitment therapy, which focuses more on let’s not change your thoughts, let’s talk about changing your relationship to your thoughts. And to me that feels a lot more affirming because it’s we’re not at all talking about let’s decide if this thought is accurate or not. Let’s talk about how it can have less power over you.
Debbie:
That’s great. Thank you for that. That’s really helpful actually to think about and it is very nuanced, but having a different relationship to those thoughts feels very different and puts a lot more control on the individual as opposed to your thoughts are dictating and running the show. Yeah, that’s great. So Debra, what do you want to say about, and again, you don’t have to go into too much detail, but because DBT is something we’ve done episodes on it and it’s really something so many adolescents are engaged in.
Debra Brause:
Yeah, I just want to add first to something Megan Anna said. I love that clarification of CBT. And I think what goes wrong maybe is when the patient’s not understanding why we’re looking at their thoughts. And they think that then they’re getting blamed, that they’re thinking what the problem is, as opposed to, like you said, the reality of the situation. They are in sort of an environment where they’re being marginalized or they’re being mistreated. And then they’re being told, well, no, it’s just the way you’re thinking about it. That’s the problem. And that’s not that’s not really what it’s meant to be saying. It’s meant to really be about, like, well, how can we look at, we hold your thoughts differently, how can we examine them and just hold them with compassion? Or, you know, it’s not meant to sort of invalidate, but I think it feels that way. I think it feels like you’re being told your thought is inaccurate.
And then that goes to like the gaslighting experience of like whatever you’re thinking is actually not real. And that can make people feel very unstable. So yeah, as far as DBT. My understanding of it is, first of all, it’s all manualized, right? So there’s all these worksheets that are given and I don’t know if this is true, but what I’ve been told is that it’s really the therapist who is deciding what the client is going to work on. There are adaptations that therapists make for neurodivergent clients, but a lot of those adaptations are just sort of pulling out certain things. Like we’re not going to work on interpersonal effectiveness, for example, which is one of the goals because that can be neuro normative. But that ultimately, it’s not addressing ruptures in the therapeutic relationship. It doesn’t really look at the therapeutic relationship. And therefore, when there is harm or when there is a client who’s having a hard time with it, that relationship doesn’t get repaired. And so I think, again, it feels like the therapist is sort of, again, the authority in the room. This person is being treated and it can feel invalidating to what their experience is. There’s also like an interesting piece of it where a lot of the goal is regulation and finding emotional regulation. And from what I heard from one particular client, it felt like this repetition of a demand to be regulated that she felt as a child. Like when instead of seeing a child through to like, we all have stress responses, they actually need to happen and they can be healthy, that the kind of bias of DBT is that we are going to regulate you and you’re going to get into your wise mind and you’re going to be calm and that can feel almost like it’s without consent. Like it’s sort of being pressured by the therapist as opposed to maybe what the client is needing. But this is just kind of what I’m taking in from the community. It’s not something I practice. So just a caveat there.
Debbie:
Thank you. Did you have any nuance to add to that Megan Anna?
Megan Anna Neff:
One just thought it activated or associated with me, in the last year, I’ve learned this framework of effect integration as an alternative to emotion regulation. And I just really love that as a framework. It’s about feeling our emotions, like feeling our way through them, integrating them into how we kind of understand ourselves. It’s a much richer, more holistic way of approaching emotions. And as someone, like I talk a lot about emotion regulation,
And once I learned that frame, I was like, oh, I really like that. It feels less mechanical, less of a demand, and more about this is a way of being with ourselves and with our emotions in a way that honors them.
Debbie:
That’s great. Thank you. So before we move on to the last portion of this extended conversation, where we’ll talk about neuro-affirming therapy and what we as parents and caregivers should be looking for when exploring different therapists, I’d love to just spend a minute talking about any potential limitations of tools like mindfulness and visualization. These are things that, you know, I remember talking to my kid once and saying, Oh, just, you know, take some deep breaths or whatever. And my child was like, everyone tells me to breathe. It is not that is not what I need to do right now. It’s like, Oh, sorry, I’m going to do the breathing. And I’m going to do what I can to co regulate with you. But I think, you know, there’s this idea that mindfulness, it works as science as it works, visualization works, but it might not be the most effective strategy for a neurodivergent person.
Megan Anna Neff:
Oh my gosh, yes, agreed. Okay, first of all, visualizations, like you’ve gotta look if the person has aphantasia, both my kids do, it’s the inability to see images. I just started asking clients about that in the last year or two before introducing anything that would be visual. Also, like if a person has a monologue, not everyone has a monologue. And a lot of therapy interventions depend on that. Mindfulness, I cannot, like, I cannot do mindfulness as an ADHDer. I talk a lot about mindfulness on the go. So, and again, this is where I do will tag my thoughts as I go. Be like, oh, right now there’s a script. Like, like anytime I do a podcast, right? There’s usually a script of like, wow, I really bumbled through my words there. And I’ll tag it like, okay, that script is plain the Bumbly podcaster, I might name it. And so mindfulness doesn’t have to be like, sit still, notice your thoughts, that’s not going to work for a lot of ADHDers. But there’s ways to adapt it where I think tagging thoughts is so empowering and so helpful, it helps contain them. I think there was a third intervention in there, but I’ve forgotten it already.
Debbie:
I think I was just saying mindfulness, visualization, breathing, and I mentioned, yeah.
Megan Anna Neff:
Oh, and breathing. So dyspraxia, I think, and just like kind of that body, awareness, body coordination can make it hard to kind of feel the sensation of a deep breath. I have found it’s kind of like 50-50 if breath works, breath work works for a lot of my folks. And that’s where, again, I’ll go back to sensory. Like, are there sensory inputs we can use that’s a little bit more concrete and tangent to activate the relaxation response? The reason the breathing works is because it activates the vagal nerve relaxation response, but there’s other ways you can do that if the body coordination breath work piece just isn’t working.
Debra Brause:
I think it’s interesting to add the body even into the breathwork sometimes. Like I remember when my kid would go to this equine therapy and they would do breathing, but they would, he would raise his arms for each breath and then raise them down. And it was like incorporating parts of the body into the breath so that it’s not just focusing on the breath because it connects to interoception as well. Right? Like if you’re not even, could be overwhelming if your internal sensations are too much or you’re just not in touch with them. So even mindfulness exercises that incorporate other senses in the breath, like touching or like paying attention to sounds or different things that can bring you into a calm state but that aren’t gonna involve being able to notice your breath because I think that can be really challenging.
Megan Anna Neff:
And be less of a demand. Like think about how many kids get told, like take a deep breath. And they’re told it often in that tone because they’re having a hard moment. And so then it’s a demand of like, you need to control yourself right now, take a deep breath. So also just taking that demand element out. I love how you’re talking about that.
Debra Brause:
Yeah. No, no, I’m thinking how that ties into all this somatic work that I think it’s so tricky because of the interoception and being able to notice what’s going on inside. The goal would be how do we build interoceptive awareness? How do we understand what’s going on inside our bodies so that we can emotionally regulate? But that is, and Kelly Mahler, who you mentioned, has a whole protocol of how to build that in, which is so cool. But it is tricky. And I think just being aware, if you’re sitting with a client and you’re asking them, like, where do you feel that in your body? Like they might not know. And that’s really frustrating. And so just being knowledgeable that, um, a lot of people have a difficult time locating feelings in their body and that that’s not that, that’s something that has to build over time, I imagine through these kinds of exercises, but it’s not something automatic. And you don’t want people to feel like they’re failing at therapy or they don’t get it or they’re not a good client. And that they might need some cognition stuff to ground them. Like that just being in the feeling experience might be overwhelming. So that sometimes bringing in a special interest or having them talk about something that they love if they’re getting overwhelmed can also be regulating. It doesn’t just have to be body sensations.
Debbie:
Yeah. That’s great. And I just want to mention Kelly Mahler’s name has come up a few times in this conversation. I did have her on the podcast a couple of months ago. So listeners, I encourage you to go back and listen to that conversation. I’ll have a link in the show notes page. So of course, my, I have so many notes written scribbled over my extensive notes that I brought into this conversation. But I do want to kind of wrap it up for at least for this specific dialogue and hopefully we’ll continue it in the future. But for listeners who have kids who are either in therapy or they’re exploring therapy for their kids and again we’re not talking about younger kids we’re not talking about OT and that type of therapy we’re talking about more I guess talk therapy I don’t know if that’s the right word but therapy for a teen or a young adult who is struggling with some mental health challenges and could use more support. What should we be looking for in order to find a therapist who would, you know, ideally do no harm with our kids?
Debra Brause:
I mean, for me, it’s starting with someone who is truly affirming in the sense that they’re not looking at neurodivergence as pathology, but as a different neurotype and as a different way of being. So you’re looking for someone who’s not using words like ASD in their bio and is not using some kind of DSM terminology or pathology to describe what they’re doing, that they’re really taking your kid in as another human that they want to get to know and learn about and kind of help them grow and develop. And that they’re also open and sensitive to, someone’s sensory needs, that they’re there to create a positive self identity for the client, that it’s about learning how to be the best version of yourself and feeling embraced for who you are someone who, you know, something I learned from Megan, Anna, like therapy can be like, we assume that people know what therapy is, but I think it’s like when it’s explained, also someone who’s going to be really clear with your kid, with you as a parent, like what are, what is the frame of therapy? What’s it going to look like? I think it can be really containing. And not just assume that the client’s going to know what they’re supposed to do, because that can be anxiety provoking. But ultimately for me, it’s the personality of the therapist, like someone who is humble, who is willing to acknowledge their own limitations, who wants to learn, and who is going in there kind of wanting to learn who your kid is or who you are as an adult and not assume that they know. And just take on a stance of like, I’m here to help you be your best self, figure out who you are, be a relational partner with me, we’re going to figure this out together, but I am not the authority on your experience. And that it’s more of a mindset, I think that’s most critical for me.
Megan Anna Neff:
I love that I often kind of land in the same place. Like, I think there are some theoretical orientations that are a little bit more, like work well with our brains. But at the end of the day, I think it comes back to the personality of the therapist. curiosity and creativity, I think would be the two elements I’d really hope for in a therapist for one of my children or neurodivergent children in general, you know, the therapist that I ended up doing really good work with, about neurodivergence until I discovered it. And then we, and then I taught him a lot, but that was the thing when I sent him a huge document about autism and autism and like non-stereotypical presentations, he read it. He was curious. We became part of our conversation. So a therapist who is, who is curious. And then I creative because, because we do often like, we’ll hit kind of interesting blocks and then we’ll have to rethink like, okay, maybe if we add drawing here, if we add an object around this conversation, maybe if we bring in D&D characters, it takes a creative therapist to be able to work with blocks that might show up and then find ways to access the inner world, especially of an autistic human. I think, again, this is an ideal situation. There are directories growing of neurodivergent therapists. I have, I’m happy to share several and we can link them in the show notes. If you’re able to find a neurodivergent therapist, that’s not just a therapist who’s gonna understand their mind, but that’s also a chance to be in relationship with someone who like who’s of their neurotype of their neurology, and who can also kind of be a model in that sense. And I think that’s incredibly powerful. That is not always available. But when you can find a neurodivergent therapist, I think that is really powerful.
Debbie:
So helpful. And so I’m just highlighting the words that jumped out at me. Humble, which I love the inclusion of that. Curious, creative, and I want to throw in the word respectful. I think it’s so important that our kids who often don’t feel respected in so many spaces feel respected by whoever they’re engaging with. So OK so much that we got into. And I just want to say, please, listeners, go to the show notes page because both Meg and Anna and Debra write about this stuff. Like, there’s a lot of resources that I’m going to put in there, including the Neurodivergent Affirming Therapist directories, which I’ve accessed. And it’s exciting to see that there’s more and more people who are kind of putting their name into the hat and saying, I’m Neurodivergent and this is my experience. So please check out the show notes page. If you guys wanna share where they can best connect with you and learn more about your work, that would be great. Do you wanna start, Debra?
Debra Brause:
Sure, I have a website. It’s drdebrabrause.com. I’m on Instagram though I don’t post very much and I have a blog on psychology today that talks about raising a neurodivergent child.
Megan Anna Neff:
It depends how you like taking in information on Instagram. If you like visuals, go there and our divergent underscore insights. I have a website neurodivergent insights.com that has a lot of blog posts and resources up there. I also have a Psychology Today blog around neurodiverse families and be neurodivergent and then a podcast more geared toward adults but divergent conversations. It’s me and another autistic ADHD therapist talking about our experience and talking a little bit of the research and then anchoring it in our lived experience.
Debbie:
Awesome. Again, links in the show notes pages, all good resources. Listeners, I also recently had Megan Anna on to talk about her awesome new book, Self Care for Autistic People, and also we had a conversation a year ago. So you’re, this is your third appearance. So I should have some kind of a prize, but yeah. Yeah, well, we’ll see. We’ll see. I just want to thank both of you for taking the time and for being willing to get into this, I know that it’s complicated. And I appreciate how you both show up to this with your own humility and curiosity. And I just really love learning from both of you. So thank you for sharing with us today.
Debra Brause:
Thank you. I just want to say, Debbie, that your book changed my whole journey as a parent and completely changed how I work with parents and has been so transformative. And I’ve learned so much from Megan Anna as well about, I mean, her wealth of information and lived experience have been transformational for me. So just being with the two of you is really such a gift. So thank you so much.
Do you have an idea for an upcoming episode? Please share your idea in my Suggestion Box.