Natasha Daniels on Helping Kids Crush OCD

It’s been a while since we’ve talked about OCD on the show, so when anxiety and OCD expert Natasha Daniels reached out about her new book, Crushing OCD Workbook for Kids, I was excited to get into it all and pulled together a lot of questions ready to make this conversation as helpful as possible for our community. So for today’s conversation, I wanted to do a deep dive into OCD and learn more about what it is, how it manifests, signs of OCD that might be missed by parents, how to tease out when something is OCD versus anxiety or ADHD or other types of neurodivergence, and lastly, how parents can support their children if they have OCD. And of course, Natasha shared some insights and tools from her new Crushing OCD Workbook for Kids, which is truly a powerful, and easy-to-use resource for any child navigating OCD and the challenges that come along with it.
About Natasha Daniels
 Natasha Daniels is an anxiety and OCD child therapist with over two decades of experience. She combines both her clinical expertise with her lived experience, raising her own three kids with anxiety and OCD. She is the author of several books including Anxiety Sucks: A Teen Survival Guide, How to Parent Your Anxious Toddler, Social Skills Activities for Kids, It’s Brave to Be Kind, The Grief Rock, and Crushing OCD Workbook for Kids. Natasha is the creator of the website AT Parenting Survival, As well as the host of the show AT Parenting Survival Podcast and the Youtube channel, Ask the Child Therapist. Her work has been featured in various places including Huffington Post, Scary Mommy, PsychCentral, The Child Mind Institute and The Mighty.
Natasha Daniels is an anxiety and OCD child therapist with over two decades of experience. She combines both her clinical expertise with her lived experience, raising her own three kids with anxiety and OCD. She is the author of several books including Anxiety Sucks: A Teen Survival Guide, How to Parent Your Anxious Toddler, Social Skills Activities for Kids, It’s Brave to Be Kind, The Grief Rock, and Crushing OCD Workbook for Kids. Natasha is the creator of the website AT Parenting Survival, As well as the host of the show AT Parenting Survival Podcast and the Youtube channel, Ask the Child Therapist. Her work has been featured in various places including Huffington Post, Scary Mommy, PsychCentral, The Child Mind Institute and The Mighty.
Things you’ll learn from this episode
- How OCD begins and manifests in children
- What intrusive thoughts or feelings are and how they can lead to compulsions
- Why OCD is often misdiagnosed as ADHD, anxiety, or self-harm and why it’s important to receive an accurate diagnosis
- What exposure response prevention (ERP) therapy is and how it supports individuals with OCD
- What OCD with support looks like over time with helpful treatment and the development of coping skills
- The importance of early intervention in supporting children with OCD
- How Natasha’s book Crushing OCD Workbook for Kids provides evidence-based tools and strategies to help children understand and manage their OCD
Resources mentioned for OCD in kids
- Crushing OCD Workbook for Kids: 50 Fun Activities to Overcome OCD With CBT and Exposures by Natasha Daniels
- Natasha Daniels Talks about Anxiety and OCD in Kids (Tilt Parenting Podcast)
- Filmmaker Chris Baier Helps Families Get Unstuck from OCD (Tilt Parenting Podcast)
- UNSTUCK: An OCD Kids Movie (Available with Spanish, French, Russian, Greek, Portuguese subtitles and an audio description)
- Help for Childhood Anxiety and OCD with Dr. Eli Leibowitz (Tilt Parenting Podcast)
Want to go deeper?
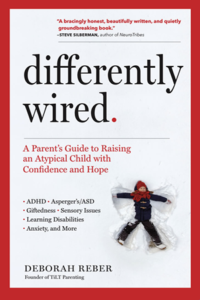
The Differently Wired Club is not your typical membership community.
 There’s something here for everyone, whether you’re a sit back and absorb learner, a hands-on, connect and engage learner, and everything in between. Join the Differently Wired Club and get unstuck, ditch the overwhelm, and find confidence, connection, and JOY in parenting your differently wired child.
There’s something here for everyone, whether you’re a sit back and absorb learner, a hands-on, connect and engage learner, and everything in between. Join the Differently Wired Club and get unstuck, ditch the overwhelm, and find confidence, connection, and JOY in parenting your differently wired child.
Learn more about the Differently Wired Club
Episode Transcript
Debbie:
Hey Natasha, welcome back to the podcast.
Natasha Daniels:
Yeah, thanks for having me back on. I appreciate it.
Debbie:
Yeah, well, I appreciate you reaching out to tell us about your new book, which we’re going to get into. It’s an excellent resource. So congratulations. It’s called Crushing OCD Workbook for Kids. But we’re going to talk about OCD today because we haven’t discussed this on the show in quite a while. And there’s a lot to get into. There’s a lot of…I think people don’t know what they don’t know when it comes to OCD and there’s a lot of ideas about what it means. So I’d like to really make sure listeners walk away with a clear understanding of what OCD means and how to support humans with OCD. Yeah, so I always do this and you’ve been your return guest, but I would love it if you just want to take a few minutes to talk about why this became a focus of your work and how it kind of weaves into your work as a therapist.
Natasha Daniels:
Yeah, I think it’s so important. Yeah, I really don’t know, to be honest. I started as a general child therapist and then I just loved working with kids with anxiety and OCD. And then after that, my kids, all three of my kids developed anxiety and OCD. It’s rampant genetically in my family, so it’s not too shocking. And I just found giving tools in a concrete way was just so rewarding. And there’s just so many things that you can do around that issue to see progress. And so I just found working with that population was the most rewarding.
Debbie:
Yeah. So you were doing this work first, and then you’re like, oh, actually, that doesn’t happen so often. I hear from a lot of practitioners who shifted their focus after the fact.
Natasha Daniels:
Yeah, it’s kind of ironic in a cruel sort of way.
Debbie:
Yeah. So, okay. I would love to just start with the definition of OCD. What is it?
Natasha Daniels:
Yeah, this actually surprisingly is not understood, I think, in the general way. OCD starts off with an intrusive thought or feeling, and then the need to do something or avoid something to get that brief relief. But the more you do or the more you avoid, the bigger the OCD grows. So it turns into this vicious circular loop. And it really could be anything. So OCD looks so different. And I think that’s where the confusion starts.
Debbie:
Yeah, because in reading your book too, I think this idea of intrusive thoughts is something we think we have an idea of what it means. But it isn’t what I think of when I think of OCD. I think of the behavior, the external manifestation of that, or what you see in the movies of someone who has OCD having to straighten things, or this kind of very specific way of navigating the world. So could you talk about that kind of difference between maybe the myth or the stereotypes of OCD versus what’s really going on?
Natasha Daniels:
So the stereotype I think is just kind of perpetuated in the media of hand washing or lining things up or being neurotic. And I mean, there are components of that. People do struggle with that in OCD, but it’s just the tip of the iceberg. It’s having an intrusive thought. Often that feels nonsensical. And so there’s an understanding often that this thought or this feeling doesn’t make sense, but there’s this itch, this need to do something to get that relief. And it can look so vastly different that I think that it gets missed. It gets misdiagnosed as ADHD or as anxiety or even as self-harm. And I think that’s why the education piece is so important for parents because often as parents, we’re part of the compulsion because we think if our child’s not over hand washing or over showering or lining things up that they don’t have OCD. But when they ask us repeatedly, I thought you were fat in my head, Mom. Am I a bad person? Or this food looks weird. Can you smell it? Or am I going to throw up today? Can you tell me I’m not going to throw up? And these reassurance questions that are like over and over and over again, we don’t realize that we are the metaphorical sink in those situations as well.
Debbie:
Oh my gosh, I already have so many questions. So I know that anxiety and OCD can be kind of maybe co -occurring, but also the anxiety might actually be OCD. But I didn’t realize that it can be misdiagnosed as something else like ADHD or maybe someone with ADHD might have OCD, but it’s not recognized. It’s just seen as part of their ADHD. Same thing with self-harm. Could you talk a little bit more about that? Because you’ve kind of really sparked me in a new way. I want to hear more.
Natasha Daniels:
Yeah, I mean, they are comorbid conditions. So somebody who has ADHD or anxiety may be more predisposed to have OCD as well, but neurologically, physiologically, they’re two very different disorders. So if someone’s having OCD, they can sometimes not focus, they’re not attending, they look distracted, they can’t sometimes complete their schoolwork. So when you’re looking at those kind of subjective ADHD testing, they can fall in those categories really easily. But it’s because they’re having intrusive thoughts, not because their brain is just randomly moving in different directions or is overly consumed with everything else that’s going on. And so that’s one area. With self-harm, there are harmful OCD themes where you get intrusive thoughts that you are concerned that you might harm yourself. And it’s scary because it’s not aligned with how you’re thinking. It’s not something you wanna do. And so you wind up asking for reassurance, you know, can you hide the knives or I’m worried that I’m sad or I’m worried that I might hurt myself. And you do need to get it assessed because you definitely want to have that. You want that distinction. You want to rule out self harm, but it is something that if a therapist doesn’t understand OCD, they may just treat it as self harm, which actually will grow the OCD because it’s validation. You’re worried about me now. I’m even more worried about me. And so it becomes a vicious loop.
Debbie:
Hmm. It’s so fascinating. You’ve mentioned this term intrusive thoughts. And again, that’s something I have an idea of what it is. And when I think of intrusive thoughts, I think of it in the context of like cognitive distortions or kind of unhelpful thinking about things. But in the context of OCD, I feel like there’s a deeper or more concrete definition of that. So what is an intrusive thought?
Natasha Daniels:
It’s hard to verbalize, but intrusive thought is, it almost feels like something foreign. It’s like a thought that pops into your head or a feeling, because sometimes OCD can be a feeling and not a thought, but that is so not aligned with you or something you hadn’t thought about to worry about. Maybe you didn’t close the door all the way and now your dog is going to get out or your family is going to be in harm’s way or maybe that thing that you said yesterday was offensive and you’re a bad person or they thought you cheated. It’s just these, and it’s different than anxiety because it’s this thought that feels so random and your brain’s like, what? Why would I think that? And then it causes distress because it’s not filtered out of the brain. And so it sits there and it causes distress. And so there’s this desire to do something with that. But there are also other thoughts, there’s intrusive feelings of this doesn’t feel just right. And there really is no core fear around that except for the fact that I’m worried that I won’t be able to ever feel comfortable. And so I have to say my words over and over until I feel just right. Or I have to write and rewrite until it feels just right. And sometimes that’s misdiagnosis perfectionism when really sometimes the goal isn’t I want to have the greatest grades or to succeed. It’s just it didn’t feel right. And so that can be a different way that it can show up.
Debbie:
I’m still so fascinated by this idea of intrusive thoughts and the overlap between anxiety and OCD. How would a parent listening know, or how would a child who has OCD know that this thought or feeling is so strong and so disconnected as opposed to this just being kind of typical anxiety, if that makes sense.
Natasha Daniels:
Yeah, normally parents and even therapists who don’t understand OCD will do the things that help anxiety and they’re not seeing any progress. And so sometimes parents will come to me and they’ll just be like, I’m so frustrated, nothing’s working. So sometimes that’s the sign because OCD is never satiated. And so with anxiety, you can reframe cognitive distortions. You can get people to look at things in a different way. There’s movement. So you’re talking to your child and we’re moving in a conversation. It’s still, I’m anxious about this, but now we’re talking about this over here. Now we’re maybe talking about this over here and there’s no stagnant feeling in the conversation. With OCD, you feel like you’re maybe even talking to the wall or to a robot because you’re repeating the same things over and over again, or you’ve rationalized with your child and it’s not helping and you’re not getting anywhere. And I always say anxiety is avoidant, OCD is bossy. So OCD wants things to happen. It’s demanding. It’s got a list of rules you have to follow or things you have to avoid or things you have to say or do. And then it hooks other people in. And so it’s more of a dictator versus anxiety, which is often avoidant.
Debbie:
And so, sorry, I’m like, I feel like I’m going off road here a little bit, but I just find this so fascinating. I’m thinking about neurodivergent humans who maybe, especially concrete thinkers who may get really stuck in their feelings, may believe all of their thoughts and feelings, right? And so, I know that traditional therapeutic modalities don’t always work very well with neurodivergent people because of that. And so I’m just wondering how would a parent know, or how could we kind of tease that out, someone who is experiencing, who’s not making progress, right, who is really stuck in that thought. So how would they go about finding out if this is OCD or should we follow, you know, that this inquiry to see if this is what’s going on? Or is this a manifestation of my child’s brain wiring and being a really rigid thinker?
Natasha Daniels:
It’s a good question because there is often like when kids are autistic, you know, the likelihood of OCD is higher as well. And so it does get tricky when we get into that world. In general, nobody likes to be on the hamster wheel of OCD compulsions. And so it is distressing. It’s distressing for the child. It’s distressing for the family. When we’re dealing with an autistic child, it is harder because there’s sometimes there’s more fusion in not being able to separate that out. Um, that maybe I just need to always save everything and wash my hands a million times a day and take showers. Maybe I need to do all that. And so it is harder to treat because there’s that other component, but often it’s, it’s distressing and it grows. And so when you accommodate it, like you might accommodate other things in the neurodivergent world when you accommodate the OCD component, it grows bigger monumentally and then it becomes more debilitating. So that becomes really apparent over time.
Debbie:
Yeah, that’s super helpful. Thank you. Sorry. I know that I’m kind of getting really nuanced, but it’s really helpful. So when we’re thinking about the compulsions that you mentioned, are those kind of, you know, I’m thinking of like a coping mechanism, right? Are the compulsions a coping mechanism for dealing with the intrusive thought? Is that really what OCD manifested is?
Natasha Daniels:
You know, I feel like we’re, we’re still behind in the science of it. And I’m not a neuroscience, but I do find the science interesting because it actually is in the same part of the brain where there’s Parkinson’s and other movement disorders, ticks, Tourette’s Parkinson’s all in the basal ganglia and the circuitry of the frontal orbital cortex. So kind of different than the world of anxiety where we’re talking about the amygdala and. And research is showing, you know, that they’re getting stuck in movement. You know, they’re getting stuck in this pattern. And so the message to the brain that you don’t need to do this or try something different or move on is not happening. And why that is obviously research is still trying to figure out the why, but they know where, you know, they know it’s the basal ganglia. And so I don’t think it’s a coping mechanism per se. I don’t know if I would describe it like that. I feel like it’s almost like a glitch. And sometimes we hear about it being described as a glitch or, um, a gear being stuck. You know, sometimes we’ll use metaphors like that because it is the circuitry of the brain and the brain is not overriding. And so when you look at MRIs, you know, the frontal lobe is all heated up. It’s like literally lighting up because it’s being, it’s an overdrive, if that makes sense. The brakes are not being turned off or they’re not being tapped. And so they get stuck on that loop and waiting for the relief and they’re not getting the relief. So they keep doing it.
Debbie:
Okay, that makes total sense. So I want to get into your book because you know, you just mentioned the gears getting stuck. And that’s one of the metaphors that you use here. And so I want to pivot to that in a moment. But if, if you could just spend a few minutes talking about some signs of OCD that parents may be seeing but not realizing, oh, this could actually be what’s going on. What are parents missing?
Natasha Daniels:
There can be so many just because OCD has so many different disguises, but normally across the board, there is a frustration of why are they doing this? If I had to summarize, it’d be like, why are they doing this? So either they are doing behaviors that seem nonsensical, opening up doors with their elbows or avoiding the couch or having to do elaborate ritualistic behavior before leaving and you know, sometimes people call it a quirk or a habit and really it’s becoming very compulsive. The other one is their involvement with you and so a lot of questions that don’t make sense or they’re not going anywhere. Some kids with moral OCD over-apologize over and over and over again or they ask questions that seem nonsensical or I think I might have like those kind of questions over and over and sometimes it’s just the acuity of these questions. On the surface, they can seem normal, but when your child’s always asking, I think I might have cheated today, and then you process that and you’re done with it and it’s not moving on, those are some signs when you’re trying to rationalize with the child’s behavior or question, and it’s like they’re stuck, they’re just repeating it.
Debbie:
Okay, super helpful. And you mentioned moral OCD, which is not something I’d ever heard of until I read your book. So that is one of the different themes that OCD, the way it can show up. So could you explain what moral OCD is? It’s not what we think of when we think of OCD.
Natasha Daniels:
Yeah, and these themes can shift and morph, but there are some common ones and moral OCD is a common one where the intrusive thought is I may have been a bad person or done bad things or I may be a bad person or I might turn into a bad person is kind of the overall arching theme. And so compulsions can look like anything, but including confessions to the parent. I think I might’ve scratched your car. I think I might’ve cheated. I think over-asking for permission, can I do this, can I do that, can I go take a shower, can I have a snack, can I, you know, can drive a parent crazy, to avoidance, you know, maybe I can’t look at billboards that have alcohol or beer, or maybe I have to hold my hands and fists so I don’t accidentally give you the middle finger, or maybe I have to avoid certain words in case I say something that’s going to offend you.
Debbie:
Okay. Well, one of the strategies that you have in your book, actually, I want before I do that, I want you to just tell me about your book. Okay. So I want to pivot and talk about your, your book, this wonderful resource that you’ve created that is actually for kids. And so kind of give us kind of an overview of what it’s all about, why you wrote it and how you hope people use it.
Natasha Daniels:
I’m really about proactive early intervention. And I feel like the IOCDF says it can take up to 17 years to actually be diagnosed and find an OCD therapist. And so many kids are having OCD signs and are not getting the right help until they’re adults. And so my hope in creating a workbook was that it was going to be this evidence -based therapeutic tool that is a good standalone or supplement to therapy, and that it would walk a child or a family through all the steps that I would have done in therapy with them. And that explains it in a simple, engaging way that they’re able to help themselves because there’re so many barriers to care that having a roadmap out there in the world that’s affordable and easy to access, I thought could be a supplement for everyone.
Debbie:
Yeah, it does feel very accessible. I think about my child’s 19, so we’re kind of past the age of doing kind of workbooks like this. But I think about the workbooks that we did together many years ago about how emotional regulation and how to tame the angry monster and how to deal with frustration and big feelings and things. And they always felt kind of cumbersome to me and hard to navigate. And your book felt so doable. It was just like, here’s a concept. I don’t know. The way that you unfolded it, it was like, this is really doable. It’s gettable. And it just feels like, OK, you can leave. I don’t have OCD, but I felt very inspired by all the strategies that you’re offering and the framework to really help kids feel empowered.
Natasha Daniels:
Oh, good. I’m glad to hear that. That was my hope. I didn’t want it to be like a heavy workbook. As a therapist, I’ve seen heavy workbooks and I know from my own experience that they don’t do them. And so I wanted it to be light. I wanted them to just be able to get through it. I could show it to my kids who have OCD and say, do you get this? And they’re like, yeah, this is great.
Debbie:
Yeah. Yeah. Yeah, there’s so much great content out there for young people. But if they’re not going to read it, what’s the point? So yeah, so I think you did a great job with it. One of the things that you talk about in the book that I really liked is to name OCD. You call OCD Mr. O for the purposes of the book. Again, I think we had the mad monster kind of externalize this presentation when my kiddo was quite young. As I was reading that, it made me think about, is there a place to be compassionate to one’s OCD? Like, it seems like OCD and Mr. O is presented as this thing that we need to be strong against that isn’t helpful for us. And I totally get that. And I don’t know, part of my brain was like, is there, is this just misguided help? Like, is there a way to be soft and compassionate to that side as well?
Natasha Daniels:
You know, that’s a great question because I think when we’re approaching anxiety, I’ll often talk about it as, you know, the over-reactive lifeguard, you know, that he’s just trying to help and he just thinks everything’s an emergency and we have to tone him down. And that works really well with the amygdala and that analogy. I still like to fight my anxiety and I kind of personify it like I’m going to crush it, but that’s my style. But I can see where it’s really beneficial, especially for some sensitive kids. With OCD, it’s super tricky because OCD will tell a lot of people, I’m just trying to keep you safe. I’m just here to be your friend. I’ve got your back more than anyone else. Don’t listen to your therapist. Don’t tell them that one part because that’s not, they’re not gonna get it. And so it is a little sticky to befriend OCD. It’s much better to say this is your basal ganglia. It’s a glitch in the brain. And the beautiful thing is we can rewire your brain. There are so many positive aspects of having OCD. And I do try to highlight that in the book. And I talk about that with my own kids, that you’re more detail oriented and you notice things other people don’t. And there’s other things physiologically that are beautiful because you struggle with OCD that we wouldn’t want to get rid of. But we don’t want to ride those neural pathways and grow a six lane highway in your brain to fuel this glitch. And so when I see it as a mechanical struggle, I feel like that is actually more scientifically accurate and doesn’t give OCD a little wiggle room to be like, aw, don’t crush me. Because OCD is like chess and anxiety is like checkers. OCD will use your tools against you. And so it’s super tricky.
Debbie:
Yeah, I appreciate that. So it seems to me in reading your book and what we’ve been discussing that there are some kinds of specific challenges for parents raising kids with OCD that are different from other things we might be dealing with. So what is the trickiest or a few of the trickiest aspects for parents whose kids have OCD?
Natasha Daniels:
I would say the hardest part is that your intuition tells you to reduce your child’s anxiety or their discomfort around whatever is happening. And that’s just our paternal or maternal instinct. And unfortunately with OCD, the more we do that, the bigger it grows. And so OCD will hook us in and have us do things to follow OCD’s rules or to do what OCD wants. And our child will be so distressed and will just be like, just do it, just say those words or just, you know, hold it for me or just tell me it’s okay or just wash this. And the hardest part of OCD treatment is systematically pulling back and detangling yourself from the OCD compulsions. And I know firsthand that’s really hard. And so there’s a lot of work that has to happen before we can do that. And you have to believe in, if I don’t be part of the loop, I’m actually helping my child. Even if my child’s OCD is saying, you’re not, and you’re not helping me, I want you to do these things. You have to believe that you’re taking the right steps, which can be really tricky.
Debbie:
Yeah, I can see how it would be kind of counterintuitive yet that idea of we don’t want to build a six lane highway as soon as you said that I got it. And a six lane highway is a lot harder to dismantle than a country lane, right? So this is important work. So besides kind of going through the workbook, with your kids, what would you encourage parents to do as kind of if they’re listening to this conversation and they’re like, Oh, I think this might be going on. What would be some of the first steps that they would take in supporting their kid?
Natasha Daniels:
Definitely get an assessment. I think if you can get an assessment by a pediatric OCD therapist, that’s important. If you even have a suspicion that you might be dealing with OCD, it’s really helpful to get an assessment. You can always get an assessment and then just leave it at that. It’s important to find someone who specializes in OCD. So I always tell people to go to the International OCD Foundation at iocdf.org/findhelp. And they have a directory there. They don’t vet out their therapists. Anyone can join that directory, but the fact that they know IOCDF is like, that’s a good first step. And so I would seek that out for sure.
Debbie:
Okay, that’s great. And then you talk about in the book, something called ERP, exposure response prevention, can you explain what that is? And how would a parent know that their child is ready to start doing that?
Natasha Daniels:
So ERP is a type of cognitive behavioral therapy. And so not every CBT therapist does ERP, actually most don’t. And so sometimes people confuse that. They think that CBT and ERP are interchangeable and they’re not. ERP is a type of CBT. And it is a therapy where you’re systematically slowly exposing your child to the thing that triggers their OCD so they can learn how to build their OCD muscles and sit with the discomfort without scratching that edge. And neurologically, it’s just triggering that mechanism without getting stuck. And so it’s rewiring their brain. And so the beautiful part about neuroplasticity is that we can change OCD by doing ERP. And that’s a wonderful thing. We don’t start off with that though. I mean, that can sound scary and we wouldn’t want parents just randomly going and exposing their child to triggers. It’s a systematic approach. That’s why you wanna get someone who is experienced in doing that or read a book that kind of walks you through it because it’s collaborative ideally. I mean, you can’t do ERP to a child. It’s educating your child, explaining what OCD is and talking about going to the OCD gym and doing these exposures systematically slowly to build up those muscles. The other thing parents can do is they can do space and the space treatment is Eli Liebowitz’s space approach of systematically pulling back those accommodations that are growing the OCD. And so there are space -trained therapists that will work primarily just with the parent. And I think that is a great supplement. And sometimes that’s a great beginning point if your child’s not at a place where they can do ERP.
Debbie:
Yeah. And in the book, I like that this is a very collaborative approach. And actually, the book is written for kids, hopefully a parent going through it or someone going through it with them. But to help them identify what’s something I could work towards, what would I be comfortable with, and how can I build this muscle and get stronger in this kind of the offense, which is something you talk about in the book. in section four, you have, which is called Offense. It’s kind of like you’re encouraging kids to proactively build up their muscles. Part of that’s exposure therapy. I’m wondering, in the book, it’s very like, do this and then this step and this step, and it seems very kind of linear and smooth. And I imagine in practice, that’s not what it looks like. So could you maybe give us an example of maybe with an intrusive thought or something that a child is working on, what it actually looks like to kind of move through these stages.
Natasha Daniels:
Yeah, and it ebbs and flows as well. So they might not be willing to do exposures and they might be willing to do exposures. Let me think of an example really quickly. I want to pick something that’s maybe not common. Because I think it’s pretty obvious when we talk about maybe contamination type of things where I can’t touch something and then I feel like I can. We’ll take something more abstract like the moral OCD that one.
Debbie:
Sorry, I put you on the spot.
Natasha Daniels:
People get confused, how are you going to do exposures around that? We don’t want to teach kids to be bad or to be okay with bad. Ironically, any child with OCD who has intrusive thoughts about moral OCD are like the last kids that are ever going to want to lie or cheat or do anything like that because it’s so triggering. Normally, they’re just really good kids. That’s why OCD is glummed onto that. But an exposure might be, we’ll talk about, I’ll use my son as an example. He’s got a little moral OCD and so there’s a collaborative approach of, and actually he was able to recognize this, hey mom, every time I say I’m sorry a lot, it’s actually my OCD talking. We call it squishy. So he’s like, that’s squishy talking. And so I’ll say, okay, well, I appreciate you letting me know that because I actually missed that one. And he’s like, so from now on, when you say I’m sorry, what would be an okay response? So this is defense, right? This is how I’m going to respond. And so we’re even coming up with a plan on defense. Well, if I say I’m sorry, just say I’m sorry is not accepted. That will drive my OCD crazy.
And so that was our plan. So now we do that. He’ll say, I’m sorry. And I feel really, I do actually feel really bad, but I’ll say, sometimes I’ll do it in an accent just to be funny. I’m like, sorry, not accepted. You know, we can make it funny. It doesn’t have to be serious. Um, and sometimes he’ll laugh and sometimes he’ll walk away frustrated. Um, but then we might do something, um, like an exposure where his OCD says he can’t, he has a lot of weird rules. Like he can’t have an iPad in public. And I noticed even recently, I can’t say the word iPad in public, like get your iPad or you can watch your iPad because his OCD says that’s a bratty thing and bratty means he’s bad and bad is bad. So we go back to that. And so an exposure might be, I’m going to bring your iPad with you. We’re at the airport and you’re going to take it out on purpose and sit with it. So it really could be anything for a child that has intrusive thoughts about lying. Maybe one of the compulsions is to soften everything they say. So they’ll say, I think I want that. Or when they make a decision, they’ll say, well, maybe I want that or I think I did this. They soften everything without anything definitive. And so we might play a game like two truths and a lie. I’m going to say two truths and a lie about me. You say two truths and a lie about what happened today. And we can play this game of like, I spy the lie. Well, for someone with moral OCD, that’s very overwhelming. So exposures don’t have to be boring. They can be creative. They could be fun. But that’s what it would look like.
Debbie:
That’s such a good example. Thank you for that. And I’m just wondering then, you know, said that we’re rewiring, you know, our brains and doing this work is creating new neural pathways. So what does that kind of look like over time? Is this something that someone can overcome? Is it just something that people learn to live with and they know how to navigate? Because I’m wondering, if you’ve kind of dealt with certain themes or certain things, do new intrusive thoughts pop up as you get older? What does that look like long term?
Natasha Daniels:
OCD is considered a chronic condition. There are flares, it does come back and so we don’t say you cure OCD, but it’s a very livable condition when you learn the skills to do ERP, you learn how to play offense and defense. And so that neuroplasticity does help reduce the symptoms. The goal isn’t to really reduce the intrusive thoughts. A lot of people think that that is the goal, that would make sense, but we can’t control what thoughts we have. But when we don’t scratch the itch, ride that six lane highway, then the loudness of it and the acuity of it goes down. And over time, it can become this annoying flea that you barely ever notice. And then there’s spikes during transitions or stressors or physiological changes or hormone changes. Life trauma can bring those things back or it just happens. And infections can bring it back. Lots of things can bring it back. And then those skills are still there. You just tap into those skills and you work on it again and it becomes kind of a lifestyle.
Debbie:
Mm hmm. That makes total sense. Just like someone with anxiety would understand this is what works for me. This is how I support myself. These are the situations that tend to trigger my anxiety. Yeah. So last question, I’m just curious to know how kids feel when they realize this is going on. I would imagine there’s a little bit of relief to know that this is something that’s happening in their brain, that it’s not that they aren’t indeed a bad person, even though that may be bad, hard for them to believe. So yeah, could you talk about that when you work with children, when they really realize and come to terms with this is how this is what’s going on in my brain.
Natasha Daniels:
There’s so much relief for so many kids because a big part of OCD is shame and embarrassment, thinking they’re crazy. And the intrusive thoughts can be so taboo or so out of left field that you’re not hearing about it. And so it’s not something that a child’s hearing at school or they think OCD is hand washing and people kind of perpetuate that. And so to sit across from a child and say, Oh, do you have these thoughts or yeah, I’ve heard this before. You know, this is, this is actually just three people ago. They were talking about the exact same thing. The relief that I’ve seen on kids’ faces, like that’s actually a big therapeutic component is just normalizing it. And that’s why I want to spend a lot of time in the beginning of my book doing that because when kids realize they’re not alone, I almost feel like that’s half the battle right there.
Debbie:
Mm hmm. Yeah. Yeah. So before we say goodbye, there’s so much in your book that we didn’t get into because I wanted to also just talk about OCD in general. What would you want listeners to know about this resource? What are you most excited about in terms of getting it out into the world?
Natasha Daniels:
I think the wait and see approach for OCD is really dangerous. And I think there’s too many people that will tell parents to have a wait and see approach. Well, it’s a little, it’s, you know, it’s OCD tendencies or I’m not sure. And I think as parents to arm ourselves with tools that we know are evidence -based and that are therapeutic is really important because the earlier we can get our kids the support and the tools, the better they’re going to feel long -term when they hit a bump and they’re like, I have these tools and they’re more innate. The younger they are, the more innate they become. It’s just part of who they are. And so that’s my hope that parents can have this in their back pocket.
Debbie:
Yeah, that’s great. Well, it’s a wonderful resource, as I said, congratulations on getting it out into the world. And would you let listeners know where they can find you and check out your podcasts and your other resources?
Natasha Daniels:
Yep, they can find me on social media at atparentingsurvival or at atparentingsurvival.com.
Debbie:
Awesome. And listeners, as always, I will have links in the show notes page, as well as a link to the conversation that Natasha and I had a couple of years ago now on the show. So that was a good listener as well. Go back and check that out. Natasha, thank you so much. I’m really happy to have had this conversation. And congratulations again on this amazing resource.
Natasha Daniels:
Yeah, thanks for having me, I appreciate it.
Do you have an idea for an upcoming episode? Please share your idea in my Suggestion Box.