What is RSD (Rejection Sensitive Dysphoria)? Dr. Norrine Russell Explains

Have you every heard of RSD or Rejection Sensitive Dysphoria? If not, or if it’s on your radar but you aren’t exactly sure what it is or what it looks like, this episode is for you. As my guest Dr. Norrine Russell explains, rejection sensitive dysphoria is commonly experienced by people with ADHD, and it can be a particularly challenging profile to recognize, understand, and support.
In our conversation, we talked about what rejections sensitive dysphoria is and how it’s different from mood disorders or emotional dysregulation, what the early signs are and examples of what it looks like, and how to support children with RSD. If you’ve ever wondered what RSD is, I know this conversation will resonate and bring value to you and your family.
About Dr. Norrine Russell
 Dr. Norrine Russell is the founder of Russell Coaching for Students, which uses an innovative method of coaching for complex students, including those who are 2E; have ADHD, Autism, or Anxiety; and those with learning differences. This innovative method, Connected Coaching, has proven successful for hundreds of students since 2009. She is the author of the recently published guide for parents, “Asking the Right Questions Before, During, and After Your Child’s ADHD Diagnosis.”
Dr. Norrine Russell is the founder of Russell Coaching for Students, which uses an innovative method of coaching for complex students, including those who are 2E; have ADHD, Autism, or Anxiety; and those with learning differences. This innovative method, Connected Coaching, has proven successful for hundreds of students since 2009. She is the author of the recently published guide for parents, “Asking the Right Questions Before, During, and After Your Child’s ADHD Diagnosis.”
With twenty years of experience creating positive youth development and parenting education programs, Dr. Russell has extensive knowledge of child development, learning styles, special needs, and positive parenting philosophies. She blends this knowledge to provide students and parents with comprehensive support and the tools they need to grow and thrive.
Things you’ll learn from this episode
- What rejection sensitive dysphoria or RSD is and how it presents
- What the early signs of rejection-sensitive dysphoria are and examples of triggers for children and adolescents
- The difference between RSD, mood disorders, and “typical” emotional dysregulation that neurodivergent children might experience
- How to support children with RSD
Resources mentioned for Rejection Sensitive Dysphoria (RSD) & ADHD
- Dr. Norrine Russell via telephone: +12127161161
- Kids in the Syndrome Mix of ADHD, LD, Autism Spectrum, Tourette’s, Anxiety, and More!: The One Stop Guide for Parents, Teachers, and Other Professionals by Dr. Martin Kutscher
This Season’s Sponsor: Fusion Academy
Is your family’s school year not going as you’d hoped? Does your student go unseen or get under-served in a big classroom? Well, I’ve got great news for you. Fusion Academy is a private middle and high school with 1-on-1 classrooms customized to your student’s pace – academically, socially, and emotionally. Fusion has more than 80 campuses across the US, along with their virtual campus, Fusion Global Academy, which serves students online worldwide. My teen attends Fusion and it has truly been a game-changer for our whole family in the best possible way.
Learn more and experience the world’s most personalized school with a free trial session at FusionAcademy.com/Tilt.
Episode Transcript
Debbie Reber 00:00
Tilt Parenting is proud to partner with Fusion Academy this season. Fusion Academy is a private, middle and high school with one on one classrooms to meet students exactly where they’re at academically, socially and emotionally. Learn more about the most personalized school in the world and how they’ve changed the lives of 1000s of families, including mine at fusionacademy.com/tilt.
Norrine Russell 00:23
Those of us who have kids who have RSD, we know what that’s like, right? They’re screaming back at you. They’re saying nothing will help. It doesn’t matter. Everyone hates me. This is the worst thing in the world. I can’t believe you’re expecting me to cope with this. Of course, I can’t cope with this. Those are some of the differences in I think how parents come to identify like, Oh, something more is going on then a temporary sadness and disappointment.
Debbie Reber 01:03
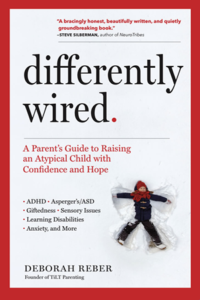
Welcome to Tilt Parenting, a podcast featuring interviews and conversations aimed at inspiring, informing and supporting parents raising differently wired kids. I’m your host Debbie Reber and I am really excited to bring you this conversation with Dr. Norrine Russell on a new topic we haven’t covered before on the show, and actually one that only came onto my radar last year, and that is rejection sensitive dysphoria or RSD, a dysphoria commonly experienced by people with ADHD. Norrine is an expert in ADHD and is the founder of Russell Coaching for Students, which uses an innovative method of coaching for complex students, including those who are 2e, have ADHD, autism or anxiety and those with learning differences. She’s also the author of the recently published guide for parents, Asking the Right Questions Before, During and After Your Child’s Diagnosis. In our conversation today, Norrine and I talked about what rejection sensitive dysphoria is and how it’s different for mood disorders or emotional dysregulation. We also talk about what the early signs are and what it might look like to an outside observer, and how to support children who have RSD. I’m sure this conversation will resonate with many of you and I hope you find this new topic interesting and valuable to your family. Before I get to that, if you haven’t yet taken my Differently Wired Seven Day Challenge, I invite you to join 4000 other parents and caregivers and sign up. You’ll get a two minute video from me every day for seven days highlighting one practical, actionable thing you can start doing right away to make a real change in the way you think, feel and act in relation to your child. You’ll also get a mini downloadable workbook to keep track of your progress. And again, it’s totally free to sign up visit tiltparenting.com/sevenday. And one last thing if you like this podcast, please help this show connect with more listeners who would benefit by subscribing and leaving a five star rating and review on Apple podcasts. Thank you so much. And now here is my conversation with Dr. Norrine Russell about rejection sensitive dysphoria.
Debbie Reber 03:20
Hey, Dr. Russell, welcome to the podcast.
Norrine Russell 03:22
Thank you for having me. I’m delighted to be here actually,
Debbie Reber 03:25
Before we get into this topic, which I’m excited about because it is a new topic for the show. But I always ask my guests to introduce themselves. In their own words, tell us a little bit about who you are. And as part of that your personal why for the work that you do.
Norrine Russell 03:40
So I’m a mom of two children ages 12 and 14, both neurotypical great kids, amazing kids, smart kids have taught me so much about life. They’re just great, great kids. My original degree is in developmental psychology. And so I’m not a clinical psychologist, I taught at a few different universities for a while, didn’t really find that to be exactly my jam. As they say, these days, I did nonprofit work for several years, which I loved. And then when my son was born, he was very complicated. And that’s when I started the coaching practice, which at the time, I kind of thought, oh, coaching is so hokey and unscientific. And that’s not what I want to be doing. But 14 years later, I’m really proud of the work that we’re doing and the ways that we’re helping families, especially because there are so many families out there who are hooked into so many different services but we’re still really not getting what they need. And so, the coaching model that we have really takes no account, what is the science of the various digital quarters of the kids that we work with, and then what is called for from a scientific point of view. So, at this point, I would say that I’m very proud to be an ADHD and academic coach. But that certainly wasn’t the case 14 years ago.
Debbie Reber 05:19
Can you say a little bit more about what’s at the core of the work that you do, you know, as a coach working with ADHD, and supporting families who are dealing with ADHD, what’s kind of at the heart of the way that you approach your work.
Norrine Russell 05:33
Almost all of the students at our practice have ADHD, our particular specialization is that we work with kids who have ADHD, autism, and anxiety, of course, we have other things. So you have learning disabilities, you know, you have depression, but almost all of the kids that we see have ADHD. And the niche that we’ve carved out really is complex ADHD. So it’s kids that have ADHD plus one or two more things. And so that might be that they have autism, it might be that they’re gifted, might be that they have a mood disorder. But for the last 14 years, we have been working with kids with ADHD. And what we really follow is what the American Academy of Pediatrics says in their 2019 White Paper, is that multi modal treatment is what’s best. And so what I see a lot of is that we take a look at this kid, we see they have ADHD, and we try to throw on all these interventions onto this individual child. Whereas really, what we need to be looking at is the context around the child, we need to be taking a look at what parent education and training and therapy is happening. We need to be taking a look at what’s really happening at school, and is it really being effective? And yes, are schools so incredibly stretched thin? Yes. 100%? Do they still have a legal obligation to these kids? Yes, they absolutely do. And then of course, medication is first line treatment for kids with ADHD. And then it’s skill building is the last part of it. And so that’s really the model that we follow. And that’s the model that’s echoed also by the American Psychiatric Association for Child and Adolescent Psychiatry. So we don’t do anything really revolutionary or out of the box, what we try to do is to apply with fidelity, what research and science has already told us works for kids with ADHD, which as you may already know, entails helping parents to let go of a lot of incorrect information about ADHD.
Debbie Reber 08:07
Absolutely. I love that you were also looking at what you refer to as complex ADHD. And I’m thinking like ADHD Plus, my hunch is, and I’m curious to know if this is what you’ve found. But would you say that the majority of people who have ADHD have something else going on? It seems like there’s a lot of comorbidities here?
Norrine Russell 08:30
No, you’re absolutely right. So the estimates are that 30 to 40% of children diagnosed with ADHD have only ADHD. Now, I would imagine that’s an under-representation Because if you get, for example, a diagnosis from the pediatrician the pediatrician isn’t going to do the learning evaluations. If you get a diagnosis from the neurologist, they’re not necessarily going to do the learning things either. And so what we for sure know is that most of the time, well, over half the time, a kid who has ADHD also has at least one other thing going on. And for a significant minority of them, they have two or three or four more things going on. My own son is a perfect example of that, where we call it the bucket full of diagnosis. He is the epitome of the kid in the syndrome mix. There was a book out several years ago called Kids in the syndrome and it was like, Okay, what do we do with these kids who have all of these different disorders, and we have to somehow sensitively, take a look at how do we create a treatment And that takes into account all of the different diagnoses and all of the different symptoms that having lots of different psychiatric disorders can create. And it’s taught.
Debbie Reber 10:17
Yeah, so complicated. I love that bucket full of diagnoses. I have not heard that one before. That’s one of the reasons why I’m so excited about this conversation today, because we’re actually going to tease out and focus on one diagnosis or one challenge that seems to be pretty prevalent in people with ADHD. But I think people don’t have to have ADHD to also have this. And what I’m talking about or teasing is rejection sensitive dysphoria, which is something that only came on my radar a few years ago, I’ve been reading more about it. It’s absolutely something I know affects many listeners of this show and what’s happening with their kids. So just to get started on that topic, could you define what rejection sensitive dysphoria or RSD? Is?
Norrine Russell 11:05
Sure, sure. So the way that people are commonly thinking about RSD right now is that this is a neurological response to some kind of rejection or conflict, that is out of scale with what is happening. Now, what’s important to keep in mind is that it’s out of scale to someone who doesn’t have RSD. But it is so real, and feels so threatening and so difficult to someone with RSD. And so basically, what it’s going to look like to someone who doesn’t have RSD, is it’s going to look like an overreaction to not getting invited to the party, or it’s going to look like an overreaction to the teacher said you need to work a little harder on this, right. But what it really is, is a neurological reaction that is intense and is frightening and is scary. And is very, very real for the person who is having the rejection sensitive dysphoria episode. And it can happen about any number of things, it can happen, because of social situations like I didn’t get invited to, you know, this party. And so nobody cares about me. And then that sort of spirals for a couple of hours into really intense negative thoughts about oneself about one’s worth wildness, and it looks like from the outside, a complete emotional meltdown about something that, again, from the outside, shouldn’t be able to be handled. But that’s not the way the person with RSD is experiencing it. And so it’s so important today that we make this differentiation between what it looks like maybe from a parent point of view, or from a teacher point of view? Versus what does it feel like to the person who is having this episode of rejection sensitive dysphoria?
Debbie Reber 13:51
It is so complicated as you describe that because I can imagine and I’ve been in conversations with other parents who talked about things that seems like their child is just being overly sensitive, or you know, and that this is part of navigating life as a human in this world means you have to toughen up or just not take things so seriously. And I think for many parents, my hunch is there’s this initial, and maybe it lasts for a long time, actually, and many parents want to explain to their kids like you’re making a big deal out of nothing, you’re gonna have to deal with this. So I’m just curious, what does the trajectory look like? What are the early signs? A parent might notice that this is actually RST. This is something significant. Is it something that a child develops as they become adolescents? Is it something you find in younger children?
Norrine Russell 14:44
I think we do see it at all ages. I think that what happens for the most part is that parents go through what is a normal rational response. to seeing an episode of RSD Oh, you need to learn to cope, you need to learn to toughen up, let’s figure out how to breathe. Let’s take some time out, let’s go for a bicycle ride, right? Like you practice all of these good coping skills, because what you want as a parent, of course, is for your child to be able to cope with the things that are difficult in life. And we know from the other piece of research that it’s very important that these sort of blips on the horizon, if you will, these challenges. These are the things that create resiliency in many kids, right? Like, oh, I didn’t get invited to the party. Oh, okay. I sit and I talk with mom at the counter. You know, maybe I have a cookie or two, maybe I have some nutritious snack and I talk through, how does it feel like why does it feel so icky that I didn’t get invited to this party, this graduation party, this birthday party, and the process of connecting with another person, the process of being listened to to the process of saying, Okay, well, what else could we do that evening that might keep you busy, and might make you feel better? When that works, then we know that we’re not dealing with RSD. Right? When the child is just really off the chain for a couple hours, and unreachable. And those of us who have kids who have RSD, we know what that’s like, right? They’re screaming back at you. They’re saying nothing will help. It doesn’t matter. Everyone hates me, this is the worst thing in the world. I can’t believe you’re expecting me to cope with this. Of course, I can’t cope with this. Those are some of the differences in I think how parents come to identify like, Oh, something more is going on than a temporary sadness and disappointment, right? My child is having an extreme reaction to the fact that the teacher looked at them wrong at school, you know, and that there’s not a way to cope with or rationalize that. That’s the time at which I think we begin to say to ourselves, oh, this is something different going on. But it’s not necessarily a mood disorder, because it’s not happening all the time, right? It’s happening in reaction to something. And that’s a perplexing part for parents to like, well, everything was just fine. And then, you know, his sister looked at him wrong, or said the wrong thing, or we asked him to clean up his room or asked him to put away his food. And all of a sudden there was this extreme reaction that was in response to what would for many children and teens be a typical, we’re going to use this word, a typical demand in their day or a typical experience in their day.
Debbie Reber 18:30
And just to clarify, because you’re talking about demands, and later today, I’m interviewing Eliza Fricker, about pathological demand avoidance, which is a presentation of autism. And that’s something very different. So we’re not talking about necessarily the demand itself, we’re talking about the way the child interprets or makes meaning out of what someone says to them, or what has happened to them or how they perceive that.
Norrine Russell 18:58
Right, right. It’s really, and this is why I think it’s so commonly associated with ADHD because many times that frontal lobe isn’t doing its job in terms of unpacking, what is the message really, you know, and I mean, and so, because that frontal lobe isn’t unpacking the message correctly, then we have this extreme emotional reaction. That’s very, very real to the person. I mean, if there’s one thing we want listeners to come away from the show, understanding is that this is a real reaction that kids are having. Now what I think is tricky about this is because there is no diagnosis for this yet and so when you try to talk to The pediatrician or you tried to talk to the psychiatrist or the nurse practitioner about this, you may be the one who’s starting to use the phrase rejection sensitive dysphoria. How much do you know about rejection sensitive dysphoria? What do you see in other kids who exhibit this kind of anger long lasting in the sense of a couple of hours, but not constant, like a mood disorder? What do you do? And this is, I think something that’s always important to me is how do we advocate for our children? You know, and part of that is asking your medical provider? Have you seen much of this before? What do you tend to do? And I think having the question at the ready, how do you differentiate this kind of what seems to be rejection sensitive dysphoria from a mood disorder, right? And then what is the treatment for rejection sensitive dysphoria? And I think asking those questions is really important, because the science of these neurodevelopmental and psychiatric disorders is very much in its infancy. And so because there is no DSM-5 diagnostic category for this, it may be that you’re dealing with a medical provider who hasn’t really heard of it, who hasn’t been to a seminar on it, who doesn’t know what they’re talking about? And they’ll say, Well, you know, these kids can be emotional sometimes.
Debbie Reber 21:37
Yeah, I’m sure that that is going to resonate with listeners too. And that is challenging, especially because we do often rely on experts to help us help our kids. And we often feel that we were kind of on the front lines of doing this research and identification, it can be challenging. And so I think a lot of parents feel insecure about their knowledge, or speaking up to experts in different areas.
Debbie Reber 22:06
And now, a quick break for a word from our sponsor. Is your family school, you’re not going as you’d hoped, does your student go unseen, or get underserved in a big classroom? Well, I’ve got great news for you. Fusion Academy is a private, middle and high school with one on one classrooms customized to your students pace, academically, socially, and emotionally. Fusion has more than 80 campuses across the US, along with their virtual campus Fusion Global Academy, which serves students online worldwide, my teen attends Fusion, and it has truly been a game changer for our whole family in the best possible way. Learn more and experience the world’s most personalized school with the free trial session at fusionacademy.com/tilt. And now back to the show.
Debbie Reber 22:57
So I wanted to ask, you’ve given a couple examples of the kinds of triggers. And I’m just wondering, you know, you said it could be like a social rejection not being invited to a party, I imagine that social piece is a big part of it, which is why I’m wondering if it is more prevalent in teens and adolescents. What other kinds of situations could potentially trigger this kind of really strong extreme response and someone with RSD?
Norrine Russell 23:24
You know, really, I think it’s anything that feels like rejection. And it’s interesting, I think, from a parent point of view, because you can have this extremely loving, extremely kind, extremely thoughtful child, and then certain things and it can be very individual to the child, come over them. And it’s like, Wait a second. Now it looks like we’re in the middle of a complete meltdown over something that really shouldn’t have in our world been so difficult, but has been difficult. I know as my son gets older, there are things like, Oh, well, he didn’t do the laundry, right? Oh, God, like, I never want to do laundry again, like laundry is stupid. I’ll never gonna learn how to do laundry, you know. And the differentiation here between kind of just a momentary frustration versus the rejection sensitive dysphoria is the length of time and the level of emotion that goes on right? We all have frustrations for sure, like, we all have frustrations, but what should be cluing a parent into, oh, is this something more is the level of the response and the length of time of the response when it takes an hour or two to recover? From the fact that the kid down the block didn’t want to share the soccer ball, as opposed to five or 10 minutes of sadness, and okay, well, let’s get the bikes out and do something else. That I think is where parents need to start thinking is this something else. And then to differentiate that from the mood disorder where the mood is kind of chronically low or anxious, it is important that there is an identifying triggering event that then provokes an hour to rage, self loathing, low self confidence. And I’m sure that, you know, if you post this question, you’ll get all kinds of examples of what it is that provokes that particular child. But from my point of view, I think it is social things. And then often, honestly, it’s teacher things, that teacher hates me, that teacher, you open up the homework at night, that teacher just hates me. And then of course, there’s the parent, you know, rejection sensitive dysphoria. You never like anything I do, nothing I do is ever good for you. You hate me, you wish I’d never been born. And that can go on and on. And meanwhile, you’re thinking, the exact opposite. All I asked you to do was clean up, you know, your makeup and your hair brushes from the counter. I think from a parent point of view, one of the things that’s so difficult is it’s a little crazy making, right? Because these are normal household requests, we won’t use the word demands, but these are normal household requests or normal household chores. And the response is so extreme that as a thinking, self aware parent, you’re thinking, Why Why am I getting this kind of extreme reaction? What did I do to provoke this kind of extreme reaction from? Could you please empty the dishwasher? Could you please put your brushes away? Could you please stand the bike up and the bike stand? You know, it could be anything. But when you’re seeing that pattern of rage for a couple hours and just inability to calm oneself down? That’s when we’re talking about what we’re calling rejection sensitive dysphoria.
Debbie Reber 27:41
Yeah, so what I’m hearing too is this perceived criticism, like a common is internalized as criticism. And I’m wondering, you’ve talked a lot about this anger, rage response. Are there other kids who just internalize this as self loathing, shame, self hatred, and go inward and have that contribute to other things? Right, like depression or other things going on? Do you see that as well,
Norrine Russell 28:09
I think we do see that. In my experience, it’s a little bit less common. But again, my experience is one professional’s experience out of 1000s, I think there are people who become very anxious people pleasers, because they never want to have that kind of rejection experience. And so everything becomes about making the other person happy all the time, so that they never get rejected. But the internal core of I’m so afraid of rejection, that that drives my every move, that’s still there, even though it may look less volatile on the outside the people pleasing mode, I think, is one possible response. But that one is harder to tease out. Because of course, you’re not seeing the outward manifestation of it, all you’re seeing is whatever you want, whatever it is that you want me to do, like, I’ll do whatever I’m supposed to do. And that one, I think, is going to be a little bit harder for clinicians to diagnose. In some ways, it’s easier to identify it when it is externalized. Now sometimes clinicians will call that that intermittent explosive disorder, well, maybe it’s not intermittent explosive disorder, or maybe the two things will end up being joined in the next DSM. You know that this intermittent explosive disorder is really rejection. dysphoria where the kid feels they’ve been rejected. And so they’re having an explosive rage experience, because they feel rejected or criticized in some way. They’re not just having rage for no reason.
Debbie Reber 30:15
So how do we support kids who have RSD? Is there a specific therapeutic approach or modality that is most beneficial or helpful for kids who are dealing with this?
Norrine Russell 30:29
I’m not a physician, so I’m not going to give medical advice. But I do want to point out that on the attitude website, that there are two possible medication solutions for RSD. The simplest solution is to prescribe an alpha agonist like guanfacine, or clonidine, and about one in three people feel relief from RSD, at the lowest possible dose of that. Another second treatment, according to Additude magazine is the ma aeoi. It’s an older form of antidepressants. And it can be dramatically effective for both the ADHD and the emotional component. I think what’s tough here is we jump to therapy as the solution. But when we are having a neurological response that is so strongly wired into the brain, we also have to take a look at what psychiatric medication can do to help with this, and then maybe there is some therapy. But the reason why things like cognitive behavioral therapy don’t necessarily work that well for rejection sensitive dysphoria, is because again, we’ve kind of lost that frontal lobe, you know what I mean? So, for many parents, the first line approach is we need to go to therapy and learn some coping skills, because this is out of control. But that is not necessarily what is first line treatment. And that’s hard for parents.
Debbie Reber 32:22
That’s good to know. And listeners, I’ll share. I know there are several articles on the attitude website about RST, and I’ll share those in the show notes too. So you can read further about those very interesting. I’m kind of mindful of the time. So I want to close this out. Is there anything that we didn’t cover about RST specifically, that you think would be really important for parents to know?
Norrine Russell 32:44
I think for parents, the challenge is figuring out what works for your child, you know, different things work for different children of different ages. And this feels awful, right? This feels awful. Is there a time period where your child needs to have some range of time? Do they need to kind of work through that in their bedroom or in a chair in the living room, and you just let it go, which I find so difficult as a parent, I want to fix it. I want to connect, right? I want to understand the response. I want to process the response. But I think figuring out as a parent, does your child just sort of need that time or they are flooded with endorphins. And they need that time and you can process it in a little bit. Is it being in the same room but not saying much? I know when my son is in an episode like this. You can’t say anything, you can’t even say, I love you. And I’m here for you. Because the rage is so overwhelming that it just provokes more rage, right? And so can you be in the same room, but quietly be in the same room? And then and then you watch right? You watch for the signs of it calming down? This breathing seems to be slower. And then you say something very empathic, that was really hard. That felt just awful. Let me know if you want to talk about it or if you want to hug. I have felt that mad before and I know how hard it is. You don’t necessarily have to say I have RST to write but you can certainly say I have felt that mad before. Or I have felt that insecure or I have felt criticized and it doesn’t feel good. And so let me know when you’re ready for a hug or to go for a walk. But I think for parents, it’s watching the clues and watching the cycle. logical and the physiological clues of when does the breathing start to calm down? When does the pacing start to slow down around the room? Do you hear the door open a little bit, you have to follow what clues the child is giving you.
Debbie Reber 35:21
That’s great advice. And I love that reminder to also just our presence, we can help co regulate, but we can just even being there can be really helpful and supportive. Before we say goodbye, I would love it if you can let listeners know how they can connect with you. And I know that you have a new book out called asking the right questions about ADHD before, during and after your child’s diagnosis. So can you tell us about that as well?
Norrine Russell 35:46
Sure. And you know what, in the second edition of the book, we’re gonna include a question about RSD. Because just being on your show has made me realize, we need to address this, this is something that we need to include in our asking the right questions . What’s the difference between a mood disorder and RSD, and emotional dysregulation? And so we’re keeping a list right now of questions for the second edition, and this will definitely be one. So that’s your original question. Our coaching practice can be found at russellcoaching.com. So two S’s and two L’s, and our phone number is 212-716-1161. I’m not sure anyone calls anyone anymore. But I always say the phone number just because if you have a question, you can also reach out on my cell phone, which is 813-508-2367. And we’re happy to help you again, our specialty is middle and high school students who have what we’re going to call ADHD plus complex ADHD. So they have ADHD, and they have something else going on. And what we’ve developed over the past 14 years is a model that tends to be highly effective. Most of our students see dramatic improvements in about a semester. And on the basis of the practice, and answering a lot of questions from parents, and teaching parents what questions to ask to be an advocate for their kid. We have written a book called asking the right questions before, during and after your child’s ADHD diagnosis. Because what we’ve learned is that parents don’t know what questions to ask, right? Your kid breaks a bone, you don’t really have to ask that many questions, right? They kind of walk you through what’s going to happen, we’re gonna get an x-ray, we’re gonna get a cast, you’re gonna go see the orthopedist, the cast is going to come off, you’re gonna go to physical therapy, there wasn’t that many questions to ask? When it comes to ADHD? There are so many questions that we need to ask. So the book is divided into before, during and after the diagnosis. And it really is a book that’s designed to empower parents to ask questions of the pediatrician, the school, the neurologists, the psychologists, the nurse practitioner, whoever it is that they see. And so the book is divided up into those three sections, we make a suggestion about questions to answer. And then each question has a resource with further information about what you should know about that question when you go in and ask the doctor like, Does my child need medication? Does my child need a 504 plan in middle school? What should I be looking at when I look at colleges for my kid with ADHD? So it’s a very practical hands on short book about what questions to ask when you have a child who potentially or who does already have ADHD.
Debbie Reber 39:15
Sounds like such a great resource. And again, listeners, I will have links to Norrine’s website and the numbers that she shared as well as this new book in the show notes page. So definitely go check those out. And, Norrine, I just want to thank you. This has been a really fascinating conversation. And again, a topic we haven’t covered before. So I’m just really grateful that you were able to share with us today and we could learn more about RSD. And what a complex complex thing it is for both kids and parents alike who are dealing with this. So thank you so much.
Norrine Russell 39:50
Thank you for having me on especially about this topic, which I think is so mystifying for parents and so hopefully hearing this podcast As we’ll help them sort out, is this what we sometimes label is bad behavior or poor coping, or mood disorder? Or is this something that we’re starting to recognize is a very particular reaction to this rejection sensitive dysphoria, and how do parents identify it and bring it to the attention of their medical and mental health provider. So thank you for having me on.
Debbie Reber 40:29
You’ve been listening to the Tilt Parenting podcast. To go deeper into this episode, visit the extensive show notes page. For every episode, there’s a dedicated page on my website with links to all the resources mentioned, a full transcript and a podcast player with key takeaways marked so you can easily go back and re-listen to the sections you’re most interested in. Just go to Tillet parenting.com/podcast and select this episode. The Tilt Parenting podcast is hosted by me, Debbie Reber, author of the book Differently Wired and the founder of Tilt Parenting. This episode was edited by Andrea Curtis-Amezquita and show notes were put together by myself, Andrea and Lindsay McFadden. If you get a lot out of this podcast and want to help cover the costs of its production, please consider joining my Patreon campaign. On Patreon you can sign up to make a small monthly contribution as little as $2 a month and it’s super easy to sign up. Just go to patreon.com/tiltparenting To learn more, or click on the Patreon link on any show notes page. To follow Tilt Parenting on social media go to @tiltparenting on Instagram and Twitter and on Facebook. Lastly, please help this podcast stay visible and easily found by the listeners who need it by subscribing and leaving a rating or review on Apple podcasts or wherever you listen to podcasts. Thank you so much. And that’s all for this week. Stay safe, stay well and take good care. And for more information about this podcast or any of the resources that Tilt offers, visit tiltparenting.com
Do you have an idea for an upcoming episode? Please share your idea in my Suggestion Box.